Cannabis for medical purposes
In Canada, and other countries around the world, CMP is an evolving area of study and course of treatment. Scientific evidence substantiating the efficacy and safety of this treatment remains limited. Anecdotally, people report that using cannabis is a natural product that helps manage symptoms for various conditions. Currently, cannabis is being authorized as a treatment for a variety of medical conditions.
Increasing numbers of Veterans are now using CMP, either because conventional treatments fail to relieve their pain or because they suffer from severe negative side effects caused by those treatments.Footnote 1
Legal access to CMP falls under the Cannabis Act, which was established in October 2018, replacing the Access to Cannabis for Medical Purposes Regulations.
Although it is legal to access CMP, Health Canada has not approved cannabis as a therapeutic product in Canada, and warns:

"the use of this product involves risks to health, some of which may not be known or fully understood. Studies supporting the safety and efficacy of cannabis for therapeutic purposes are limited and do not meet the standard required by the Food and Drug Regulations for marketed drugs in Canada."
There are a couple of pharmaceutical medications which have been developed (Sativex and Cesamet) that contain cannabinoids and have been approved for specific indications by Health Canada.
Herbal medical cannabis, such as dried cannabis and oils, have not gone through Health Canada's drug review and approval process, and do not have a Drug Identification Number (DIN) or Natural Product Number (NPN).Footnote 2

The Canadian Medical Association and the College of Family Physicians of Canada) echo this point and caution their members in authorizing CMP as a treatment.

Both the Canadian Medical Association and the College of Family Physicians of Canada note that there is insufficient evidence and clinical information on the safety and efficacy for most therapeutic claims of CMP.Footnote 3Footnote 4
That said, CMP research has shown some success with low- tetrahydrocannabinol (THC) and high cannabidiol (CBD) products. This has laid the groundwork for national health insurance providers to cover CMP for specific conditions, including:
- Pain and other symptoms in a palliative setting;
- Loss of appetite or nausea due to treatments for cancer or HIV/AIDS;
- Spasticity or neuropathic pain associated with Multiple Sclerosis;
- Spasticity due to spinal cord injury;
- Refractory pediatric onset epilepsy; and
- Chronic Neuropathic Pain
Insurance providers who cover CMP do so under very controlled circumstances with limitations on quantity, cost, methods of administration, and requirements for continued monitoring and reporting.
The College of Family Physicians of Canada also states that physicians should follow the regulations and guidelines of their provincial College when authorizing CMP as a treatment. The guidelines set out by the provincial and territorial Colleges are relatively similar in nature and include:
- physicians must weigh the available evidence in support of cannabis against other available treatment options
- advise patients about the material risks and benefits of cannabis
- physicians must exhaust other possible treatments before authorizing cannabis and must document the treatments that were attempted but failed.
- assess a patient's risk of addiction using a validated addiction risk tool
The following fact sheet, shown in Figure 1, provides a basic overview of common cannabis plants and products, methods of consumption as well as information to better understand consumption and harm reduction.
Figure 1: Cannabasics, Canadian Public Health AssociationFootnote 5
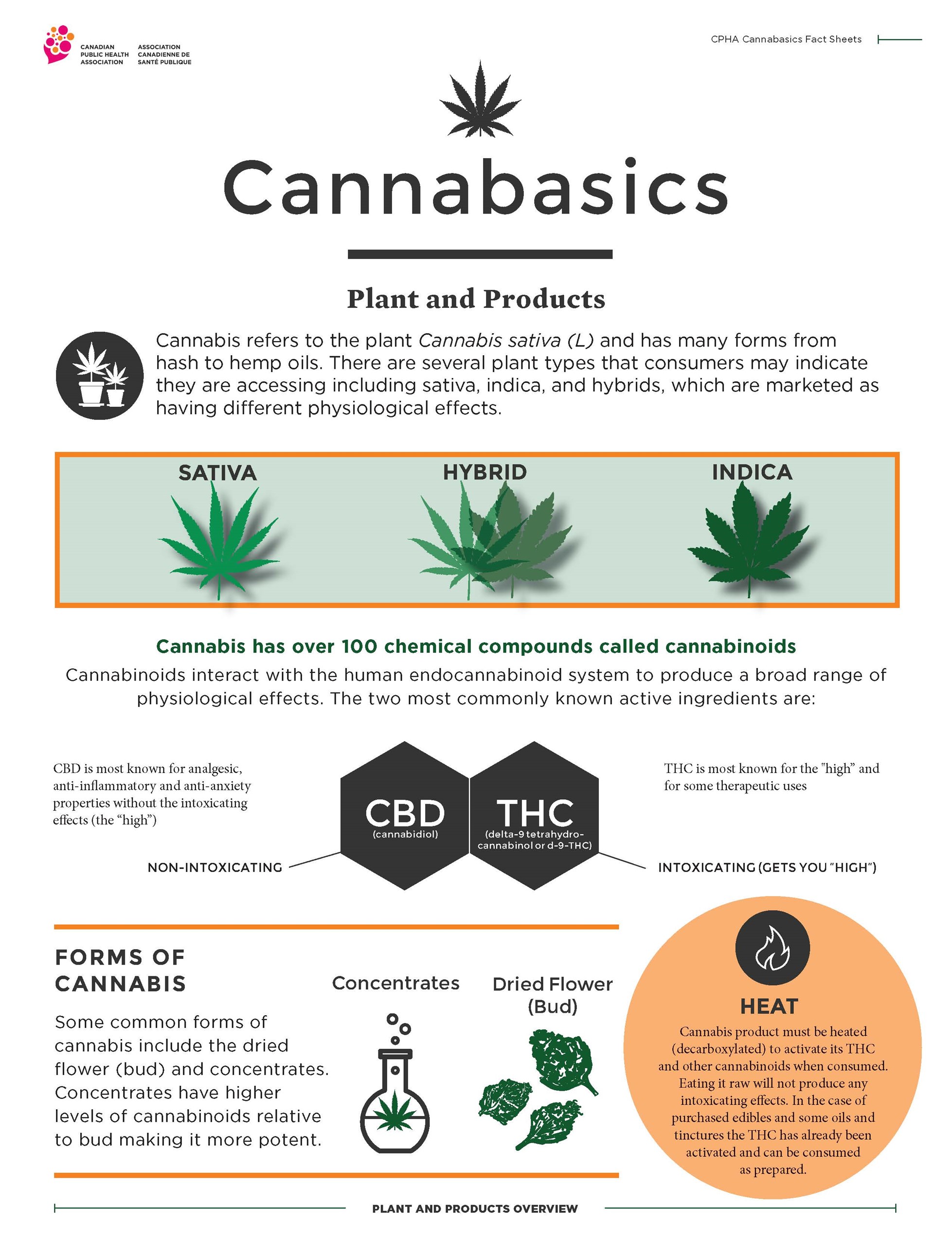
Cannabasics
Plant and Products
Cannabis refers to the plant Cannabis sativa (L) and has many forms from hash to hemp oils. There are several plant types that consumers may indicate they are accessing including sativa, indica, and hybrids, which are marketed as having different physiological effects.
- Sativa
- Hybrid
- Indica
Cannabis has over 100 chemical compounds called cannabinoids
Cannabinoids interact with the human endocannabinoid system to produce a broad range of physiological effects.
The two most commonly known active ingredients are:
- CBD (cannabidiol): CBD is most known for analgesic, anti-inflammatory and anti-anxiety properties without the intoxicating effects (the “high”) - NON-INTOXICATING
- THC (delta-9 tetrahydro-cannabinol or d-9THC): THC is most known for the "high” and for some therapeutic uses - INTOXICATING (GETS YOU “HIGH”)
Forms of cannabis
Some common forms of cannabis include the dried flower (bud) and concentrates. Concentrates have higher levels of cannabinoids relative to bud making it more potent.
- Concentrates
- Dried Flower (Bud)
Heat
Cannabis product must be heated (decarboxylated) to activate its THC and other cannabinoids when consumed. Eating it raw will not produce any intoxicating effects. In the case of purchased edibles and some oils and tinctures the THC has already been activated and can be consumed as prepared.
Benefits and risks
There is limited medical evidence for the use of CMP. However, the field of study is continuing to grow as cannabis is more used as a treatment and has also been legalized in some areas of the world.
In addition to the need for more research on CMP’s effectiveness and safety, there is currently no scientifically defined dose of cannabis for any specific medical condition. Dosing remains highly individualized and relies greatly on finding the right dose where potential therapeutic effects are maximized while adverse effects are minimized.Footnote 6
Different strains of cannabis have varying degrees of potential effects depending on the relative THC and CBD content. Both THC and CBD are associated with pain relieving and anti-inflammatory effects. However, THC may produce psychoactive effects while CBD has been linked to anti-nausea, anti-anxiety and muscle relaxing effects.
THC causes the intoxicating effects (or "high") and the impairing effects, but it can also cause anxiety and other adverse effects. CBD is not intoxicating and may reduce some of the effects of THC; however, it does have an effect on the brain. Higher levels of THC can cause greater levels of impairment and increase your risk of experiencing serious adverse effects.
The College of Family Physicians of Canada guidelines on CMP recommend that an authorization for a CMP product that contains THC should also have CBD in it to balance out the psychoactive effects. They go further to note that for smoked cannabis, "original doses should be at most nine percent. THC (with appropriate CBD) at doses of 0.4grams to 0.7 grams per day. If the THC percentage increases, the gram dosing should be decreased appropriately."Footnote 7
Concerns have also been raised by the Canadian Centre on Substance Use and Addiction. Despite its legalization and promising research for its medical application, regular use of cannabis can lead to adverse health outcomes. Regular cannabis use can affect mental health; cognitive functioning, including attention and memory; as well as respiratory and cardiovascular health. Also noting that regular cannabis use can increase the risk of developing psychosis and schizophrenia.Footnote 8
The Centre also acknowledged that it is presently not clear on the extent to which regular cannabis use leads to depression or anxiety, after accounting for common factors (e.g., socioeconomic status, alcohol use etc.). However, problematic cannabis use and cannabis use disorder is more common among individuals with mood and anxiety disorders compared to those who are not experiencing these conditions. Regular cannabis use is generally associated with more harms than benefits among individuals with mental health conditions.Footnote 9
Ultimately, it is critical that health care practitioners authorizing the use of CMP as a treatment weigh all of the risks with the potential benefits. Extensive education and rigorous follow-up care are essential to quickly identify if the treatment stops working as intended. Follow-up care is also needed to identify and address negative side effects that can hurt a patient’s long-term rehabilitation.
The equivalency factor
Oil, edibles, extracts and topicals: How does it all weigh up?
The equivalency factor is based on the quantity of dried cannabis that is required to produce 1 mL of cannabis oil.
The formula for converting dried cannabis into oils, edibles, extracts or topicals are often considered proprietary in nature by a Federal Licensed Seller based on the specific product.
When processing a CMP order, the Federal Licensed Seller will use their formula to deduct the equivalent of dried grams of cannabis based on the client’s authorization.
However, there is a gram equivalency that the government of Canada uses to identify possession limits based on weights.
For example:
1 gram of dried cannabis = 0.25 grams of concentrates (solids or liquid)

Accessing cannabis for medical purposes in Canada
Canadians wishing to purchase CMP must adhere to the Cannabis Act and Regulations. Under these regulations, the general process to purchase CMP is as follows:

A patient meets with their healthcare practitioner to discuss whether CMP is a good treatment choice.
The healthcare practitioner (a licensed physician or nurse practitioner) provides them with a formal “medical document” which is the “authorization” for the patient to access CMP from one of Canada’s federal licensed sellers.

Once the patient has the medical document (i.e., the authorization), they register with a federally licensed seller(s). The medical document is sent to the federal licensed seller and kept on file.

Once registered with a federal licensed seller, the patient can order product and have it delivered.
Interestingly, other than authorizing the number of grams/day, the medical document template provided by Health Canada provides no details on important information such as condition being treated, the method of administration (smoking, topical oil, etc.) or the type of cannabis product. Essentially, a patient is free to purchase any product from the federal licensed seller as long as they stay within the daily dosage limit.
The Michael G. DeGroote Centre for Medicinal Cannabis Research sums this up on its website as follows: “Fundamentally, ‘prescriptions’ for medicinal cannabis are authorizations for access, not a precise identification of a controlled medication that is prepared and dispensed by a trained pharmacist. They are more like permission slips with non-binding recommendations than actual prescriptions for medications.”Footnote 10
In contrast, the use of prescription for a regulated drug would be filled through a pharmacy. A pharmacist provides a layer of oversight to ensure patients understand proper dosing information and to identify any negative drug interactions. For CMP, there is no pharmacy oversight required. Although some clients choose to go through a pharmacy service that offers cannabis, most do not.
The Canadian Pharmacist Association echoes these concerns in their independent assessment report: Improving Medical Marijuana Management in Canada.
While Health Canada has published guidelines that include available clinical evidence, potential risks, and daily use limits, there is still insufficient formalized guidance for health care practitioners regarding strains, dosages and forms.
In their report, the Canadian Pharmacist Association also noted that when protecting patient safety, “the aim should be to move the bar as high as we’d expect for any product that is used for medical purposes.” As well as the “Adoption of prescription drug-like attributes for CMP leads to appropriate controls being in place to better protect public health safety.Footnote 11
Health Canada reported that in March 2021, more than 292,000 Canadians were registered to access CMP. The average daily amount authorized by health care practitioners for these individuals who access from federally licensed sellers has remained relatively constant at 2 grams/day since the coming into force of the Cannabis Act in October 2018.Footnote 12
Cannabis for medical purposes at VAC
VAC’s mandate is to support the well-being of Veterans and their families. One of the ways this is achieved is through listening to the suggestions of Veterans, their representatives and stakeholders to guide work and research, and strive to design and deliver programs that meet the modern and changing needs of Veterans and their families.
In 2008, VAC started reimbursing for the cost of CMP on an exceptional basis to Veterans who obtained the product following federal regulations. VAC then continued to cover costs of CMP for Veterans who were approved by Health Canada through the Medical Marihuana Access Regulations based on certain categories of symptoms and conditions. In 2012, VAC implemented guidelines to help provide direction for requests of CMP as a treatment as federal regulations continued to change. In 2016, the Office of the Auditor General of Canada released a report on VAC drug benefits. The report included a recommendation for VAC to explore ways to manage the rising costs of CMP.
In March 2016, the Minister of Veterans Affairs announced a comprehensive review of CMP . The Audit and Evaluation Division’s review resulted in a report recommending, among other things, the development and implementation of a policy for CMP. VAC has acknowledged that CMP is an evolving area of treatment and that it would monitor information and continue to adjust the policy to ensure the well-being of Veterans and their families.
VAC’s policy on CMP coverage falls under the Treatment Benefits Program of Choice “Reimbursement Policy on Cannabis for Medical Purposes (the Policy) became effective on 22 November 2016. The policy has been updated to remain current with the changes to federal regulations.
The Policy:
- establishes a reimbursement limit of 3 grams/day of cannabis sold by licensed sellers or its equivalent in fresh cannabis, cannabis oil, cannabis edibles, cannabis extracts or cannabis topicals.
- outlines an exceptional approval process for Veterans seeking reimbursement for more than 3 grams/day limit through consultation with relevant medical specialists.
- states reimbursement will be made based on a maximum rate per gram of cannabis.
Veterans order their CMP directly from the federal licensed seller which then bills VAC for the cost. The Veteran is not out of pocket. VAC uses a third-party service provider to manage the authorization process and to pay these invoices.
The number of VAC clients with active authorizations for CMP has been increasing year over year resulting in a 660% increase between 2015-16 and 2019-20. Costs for CMP reimbursements have increased significantly as well. See Figure 2 for details.
Figure 2 : Historical Cannabis Reimbursement Dollars and Veteran Count


Dollars (Millions)
| 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 |
|---|---|---|---|---|
| $20.54 | $63.70 | $50.97 | $74.82 | $85.15 |
Veterans (Count)
| 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 |
|---|---|---|---|---|
| 1,762 | 4,474 | 7,298 | 10,466 | 13,270 |
Source: AED analysis based on data extracted from FHCPS system
There was a slight decrease in 2017-18 costs showing the impact of the implementation of the Policy. However, in subsequent years, this was more than offset by an increase in demand for CMP. The stakeholders interviewed have attributed the increase in demand to the legalization of cannabis in Canada in 2018 citing increased acceptance from both prospective patients and authorizing health care professionals.
VAC has two streams for Veterans to be reimbursed for CMP: up to 3 grams/day and the exceptional process for more than 3 grams/day.
- Up to 3 grams/day will be approved as long as the medical authorization lists the Veterans’ disability benefits entitled conditions (or “entitled condition”). CMP does not restrict CMP to certain conditions. CMP does not know for which condition (if there are multiple conditions) the CMP is being used to treat.
- Exceptional Process (in excess of 3 grams/day) requires additional information. The request must have a supporting letter by a medical specialist with expertise in the condition for which CMP is authorized (psychiatrist, pain specialist, etc.). The specialist is not the authorizer, they are supporting the request for the excess of 3 grams/day. The Department has added an administrative cap on the program of 10 grams/day.
As shown in Figure 3, on 31 December 2020, 60% of Veterans are receiving reimbursement for the maximum 3 grams/day, and 20% were exceptionally approved for more than 3 grams/day.
| User Group | Veteran Count | % of Total Authorizations |
|---|---|---|
| Under 3 grams/day | 2,674 | 19.4% |
| 3 grams/day | 8,395 | 60.9% |
| Over 3 grams/day | 2,747 | 19.9% |
Source: AED analysis based on data extracted from FHCPS system
VAC supported research
In 2018, the Subcommittee on Veterans Affairs of the Standing Senate Committee on National Security and Defence launched a study on Canadian Veterans’ use of CMP. Their report addressed VAC’s reimbursement policy for CMP and reiterated the consensus view that more research on the use of CMP is greatly needed.Footnote 13
VAC is working closely with partners, such as McMaster University’s Michael G. DeGroote Centre for Medicinal Cannabis Research, that continues to review and pursue study into CMP.
In 2021, McMaster University released the results of a systematic review and meta-analysis of randomized clinical trials regarding medical cannabis or cannabinoids for chronic non-cancer and cancer related pain. This research was funded by VAC. The expert panel provided a summary of recommendations and was confident that non-inhaled medical cannabis or cannabinoids:
- Result in a small increase in the proportion of people living with chronic pain experiencing an important improvement in pain and sleep quality (high and moderate certainty evidence, respectively);
- Result in a very small increase in the proportion of people living with chronic pain experiencing an important improvement in physical function (high certainty evidence); and
- Do not improve emotional functioning, role functioning, or social functioning (high certainty evidence).Footnote 14
VAC continues to assess and support the research needs in the area of CMP treatment for Veterans. The rapid recommendations that resulted from the research done by McMaster University is the starting point for the VAC-funded development of clinical guidelines for cannabis use in treating chronic pain, which will wrap up in 2024.