3.1 Non-exceptional stream (3 grams and under per day)
Veterans can easily access reimbursement for CMP through VAC’s Health Care benefits, especially if their authorization is under 3 grams a day of dried cannabis or the equivalent in fresh cannabis, edible cannabis, cannabis extracts (including cannabis oil) or cannabis topicals.
VAC currently covers CMP for any pensionable condition, even though Cannabis is not an approved therapeutic treatment in Canada. In doing so, VAC must ensure the benefits outweigh the risk to Veteran’s health and well-being, including their risks for substance misuse, substance use disorders, and related health consequences.
While there are countless anecdotal reports concerning the therapeutic uses of cannabis, clinical studies supporting the safety and efficacy of cannabis for therapeutic purposes in a variety of disorders are limited. As noted, there is no scientifically defined dose of cannabis for any specific medical condition. Dosing remains highly individualized. The current available information suggests most individuals use less than 3 grams daily of dried cannabis.
Given these uncertainties, VAC established a maximum reimbursement of 3 grams/day of dried CMP (or equivalent in other product types) when it developed its Reimbursement Policy on Cannabis for Medical Purposes (the Policy) in 2016 as a means to mitigate the potential health risks to Veterans.
For the 3 gram/day threshold to be effective, the audit team expected that the majority of Veterans would be reimbursed for fewer than 3 grams/day. We found that the 3 grams/day maximum was not effective in limiting the health risk to Veterans as shown by the low decline rates and by the high percentage of authorizations at the 3 grams/day and over at 31 December 2020.
VAC policy does not address conditions covered or comorbid health conditions
VAC has only one requirement for accessing CMP reimbursement for this group: that the medical document lists an entitled condition. Decline rates for requests up to 3 grams/day are very low. The audit determined that decline rates for this group was at most 1.9% during our scope. The low decline rates are a direct result of the fact that VAC has not restricted / mapped specific entitled conditions to access CMP reimbursement like it has for other treatment benefits.
The audit noted that insurance providers have begun to offer coverage for CMP, but for only very few conditions (none of which are mental health related) and with other limitations, such as dollar caps and the need for extensive documentation.
The Canadian Medical Association and the College of Family Physicians of Canada caution its members in authorizing CMP. In the College of Family Physicians of Canada’s guidance in authorizing CMP, they note that there is little research evidence to support the authorization of cannabis as a treatment for pain conditions commonly seen in primary care. They do suggest authorizations for CMP can be considered for patients with chronic neuropathic pain or palliative cancer pain that has failed to respond to standard treatments.Footnote 15
Percentage of authorizations at 3 grams/day and over
VAC’s CMP policy is driving behavior resulting in the majority of Veterans who apply for the benefit are receiving coverage for the daily maximum of 3 grams/day.
VACs external website questions and answers about the Policy notes that “the policy was based on the published guideline from the College of Family Physicians of Canada, that advises that, ‘...the upper level to the safe use of dried cannabis will be on the order of 3.0 g per day, and that even this level of use should be considered only in very circumscribed conditions.’”
As shown in the following table (Figure 4), at 31 December 2020, 81% of the active authorizations were for 3 grams/day or more.
| User Group | Veteran Count | % of Total Authorizations | Average Grams Authorized |
|---|---|---|---|
| Under 3 grams /day | 2,674 | 19.4% | 1.7 |
| 3 grams/day | 8,395 | 60.9% | 3 |
| Over 3 grams/day | 2,747 | 19.9% | 7.1 |
Our data analysis shows a very high correlation between an increase in the number of grams/day authorized with each subsequent authorization. If these trends continue, we will see more Veterans accessing CMP through the exceptional process, which is already high at almost 19% of authorizations. Internal medical experts have indicated that the exceptional rate should be closer to 1-2%.
Data analysis also showed that the average grams/day authorized for Veterans in the exceptional group (i.e., over 3 grams/day) is 7.1 grams which is very high in comparison to the Health Canada reported average of 2.0 grams/day for Canadians accessing CMP.
Health Canada estimates that 1 in 11 (9%) of those who use cannabis will develop an addiction to it. However, if a person smokes cannabis daily, the risk of addiction is 25% to 50%.Footnote 16
VAC’s policy does not address THC / CBD content
As noted, THC has some therapeutic effects, but it also has harmful effects. CBD is another therapeutic cannabinoid. Unlike THC, CBD does not produce a “high” or intoxication.
Experts agree that as THC increases, the health risk increases. Clinical practice guidelines are limited and evolving. VAC’s policy is silent on THC content and business rules don't require that physicians note THC on authorizations. However, the College of Family Physicians of Canada notes that “although it is not required by regulations, physicians should specify the percentage of THC on all medical documents authorizing cannabis, just as they would specify dosing when prescribing any other analgesic.”
The College of Family Physicians of Canada also recommends using the following harm reduction strategy for establishing dosage: “We recommend that initial total daily dose for oil consumption does not exceed 2 grams/day. Inhaled (and smoked) cannabis could be started at 0.5 grams/day. We recommend using the smallest effective dose and keeping the total maximum daily dose at 5 grams/day or lower.” They also note that, “while 2.5 grams to 3.0 grams a day is considered an appropriate upper limit of individual dosing, larger amounts might be required when using oils. To approximate, 1.0 grams (or 1 mL or 1 cc) of cannabis oil could require approximately 3.0 grams to 3.5 grams of dried cannabis.”Footnote 17
Without collecting and analyzing critical information about Veterans’ use of CMP, the Department cannot identify trends that may be problematic and adjust policy to safeguard the health and well-being of Veterans.
Recommendation #1:
Part 1: It is recommended that the Assistant Deputy Minister of Strategic Policy and Commemoration in consultation with the Assistant Deputy Minister of Service Delivery reviews and updates the policy for CMP with a lens for the health and well-being of Veterans. This review and update would include:
- Seeking external expert guidance on the Policy for CMP
- Updates to the policy must address guidance around:
- Conditions covered;
- Comorbid health conditions and contraindications that would affect the use of CMP as a treatment option;
- Limits on daily grams/day, as well as guidance and limits to the THC/CBD content in CMP products covered; and
- Method of administration and what types of products are covered under the policy.
- Continue to review and update the policy regularly based on the evolving research and regulations concerning CMP.
Part 2: It is also recommended that the Assistant Deputy Minister of Service Delivery update and adjust related program processes and business rules to align with policy changes.
Management agrees with this recommendation.
Since 2016, the policy has been updated four times to reflect the evolving environment associated with cannabis. Similar to 2016, external experts and internal stakeholders will be engaged to provide guidance that will inform an updated policy.
The updated policy will include more detailed guidance around the nature of conditions for which CMP will be reimbursed, daily gram limits, and the nature of products included.
Service Delivery Program Management division is committed to working with Contract Administration, the Policy and Research Division, the Health Professionals Division and the third-party service provider to support, implement and operationalize changes to the Reimbursement Policy for Cannabis for Medical Purposes.
This includes developing functional guidance, developing and delivering required training and effectively communicating changes to program processes and requirements to Veterans, the medical community, federal licensed sellers and external stakeholders.
Recommendation #2:
It is recommended that the Assistant Deputy Minister of Service Delivery develop a detailed authorization form for CMP that would allow the authorizing Health Care Practitioner to demonstrate their due diligence in recommending CMP as a treatment option for the Veteran. The health care practitioner will need to provide more specifics on the course of CMP treatment for their client’s condition(s).
This would include, but not be limited to:
- the primary and secondary conditions being treated,
- type of CMP to be used,
- method of administration and frequency, and
- the specific THC/CBD composition.
The form should note any comorbid conditions as well as previous treatments that were unsuccessful. It should also note if the authorizer is the client’s family doctor or include assurance that the information will be provided to the family doctor by the authorizing health care practitioner. The authorization form should include the plan for ongoing follow-up with the Veteran over the course of the CMP treatment.
Only the products purchased from a Federal Licensed Seller that match the detailed authorization form would be eligible for reimbursement by VAC.
Management agrees with this recommendation.
Program Management has been developing a detailed VAC authorization form to be completed by health care practitioners authorizing cannabis for medical purpose.
Service Delivery and Program Management is committed to finalizing development of this form in consultation with Health Professionals, Access to Information and Privacy, and VAC Legal Services, and effectively communicating new requirements regarding the use of this form to Veterans, the medical community, federal licensed sellers and external stakeholders.
3.2 Exceptional authorizations above the CMP limit (over 3 grams per day)
The exceptional process business rules are being followed. However, the demand for exceptional approval of more than 3 grams a day continues to grow.
Veterans who routinely take high dosages of CMP (especially with high THC) over a prolonged time can:
- result in psychological dependence (addiction),
- increase the risk of triggering or aggravating psychiatric and/or mood disorders (schizophrenia, psychosis, anxiety, depression, bipolar disorder)Footnote 18
The “exceptional process” refers to the policy enacted steps needed for Veterans requesting access to reimbursement for more than the 3 grams/day maximum. The exceptional process involves additional requirements to address the heightened risk of accessing additional daily amounts of CMP. In addition to needing the medical document to list the entitled condition, the exceptional process requires a letter from a medical specialist supporting the necessity of the additional amount.
VAC’s policy requirements are broken down into detailed “business rules” which inform the third party service provider on the detailed steps necessary to approve authorization requests and to pay invoices to federal licensed sellers. We expected that the additional controls VAC implemented for this group of Veterans would be effective in addressing the heightened risk and in supporting the health of Veterans.
The audit found that the business rules for the exceptional process were being followed by the third party service provider; however, they were not effective in addressing the heightened risk of this group. Essentially, rules have been streamlined for expediting access and are not balanced with the well-being of Veterans.
Patient Follow-up Care by Health Care Practitioners
While guidelines from the provincial Colleges of Physicians and Surgeons vary, there is a general consensus that a health care practitioner must be considerate of all previous health issues, treatments and potential risks when authorizing CMP. They also note the importance of a follow-up plan and evaluating the patient regularly.
In their guidance on authorizing CMP, the College of Family Physicians of Canada recommends regularly monitoring patients and using harm reduction strategies such as:
- When initiating CMP, establish specific and realistic treatment objectives,
- Schedule follow-up visits every four to eight weeks after initiating the treatment and as needed, or every three months when the dose is stable, and
- With regular CMP users, plan for periodic re-assessments of CMP therapy effectiveness and possibility of tapers.Footnote 19
The recommendations that came from the research conducted by McMaster University also provide insight into the importance of follow-up appointments between a patient using CMP and their health practitioner. It notes that, once a trial of medical cannabis has been initiated, unexperienced cannabis users should be reviewed at least every month until a stable dose is achieved; experienced users can be reviewed after three months.
The recommendations also explained that if benefits are limited or problematic side effects are reported, health care practitioners may choose to end treatment, adjust dosage (grams and THC/CBD content), or change the route of administration. Cannabis should be discontinued if, despite these strategies, patients continue to experience problematic side effects, a maximum dose is achieved without important benefits, or patients are diverting cannabis or develop a cannabis use disorder. If management with medical cannabis is successful, patients should be followed up (for example, every three to six months) after a stable dose has been achieved.Footnote 20
Denial rates for exceptional authorization requests
Given the potential risks to Veteran’s health and the additional measure put in place by VAC for those seeking reimbursement of more than 3 grams/ day, we expected denial rates to be relatively high. The third party provider reported that the denial rate for this group was approximately 22%. However, this rate was calculated based on individual instances of denials and was not adjusted for those requests that were denied and later approved. Audit and Evaluation Division adjusted the reported denial rate for those that were subsequently approved and noted that the actual denial rate was at most 7.8% during the scope period. Again, this low denial rate illustrates how the controls put in place to mitigate the increased health risk for the exceptional access group are not as effective as intended.
Authorizers with high Veteran patient counts
Experts agree that given the lack of evidence for efficacy and safety coupled with the lack of guidance on dosing, it is important that patients accessing CMP are under careful watch of a medical professional.
VAC’s role is to help Veterans access the supports and services they need. VAC does not interfere with the physician-patient relationship of a Veteran. VAC, however, is able to analyze the population and identify concerning areas. For example, there are small number of CMP physician authorizers with a very large Veteran patient loads bringing into question the robustness of the medical oversight. During the audit scope, out of the total 13,796 Veterans being reimbursed for CMP:
- One health practitioner authorized access to CMP for 1,294 Veterans;
- Three more authorized between 700-830 Veterans; and
- Six more authorized over 300 Veterans.
Medical Specialist letters
Medical specialists have become more familiar with VAC’s eligibility requirements. They are conscious of the requirements when designing their letters to ensure acceptance. We also noted that specialist letters show very little sign of a strong physician / patient relationship:
- Follow-up recommendations were vague, using wording such as “follow up in six months or as clinically required;”
- Just over half of the specialist letters we reviewed did not mention anything about follow-up;
- Specialists are required to list the contraindications that were considered in their patient evaluation. We noted that the contraindications information provided varied in depth and detail as some noted simply “no contraindications.” Additionally, we noted instances where the support letter would make reference in the background section to known contraindications (mental health conditions primarily) but would not list them as outright contraindications with supporting rationale that the benefits would outweigh the risks of the CMP treatment.
Recommendation #3:
For Veterans receiving exceptional amounts of CMP, it is recommended that the Assistant Deputy Minister of Service Delivery incorporate a level of assurance that the health care practitioner authorizing the treatment has provided follow-up assessments with the Veteran, monitoring their symptoms, progress and well-being throughout their CMP treatment.
This level of assurance should happen at least once between the annual renewal of a CMP authorization, and it should provide assurance that the goals of the treatment are being met, and that a mental health assessment was completed which included monitoring for signs of substance use dependency.
Management agrees with this recommendation.
Service Delivery and Program Management commits to implementing a follow-up assessment tool to be completed by the authorizing health care practitioner at intervals established in consultation with the Health Professionals Division.
This includes developing functional guidance, providing required training and effectively communicating changes to program processes and requirements to Veterans, the medical community, federal licensed sellers and external stakeholders, and collecting and reporting pertinent data.
3.3 Collection of data and trends to inform policy
VAC can do more to analyze data and identify trends to inform policy.
As the CMP program continues to mature, and the demand for the program continues to grow exponentially, the department will need to properly manage resources and examine policy and program effectiveness.
There is opportunity to improve data collection efforts such that key information is captured, analyzed, and used for policy decisions.
We expected that VAC would capture and monitor important data and trends to inform its policy regarding CMP. Important data would be on the types of conditions being treated, the type of cannabis being used, the CBD/THC content of products used, and the method of administration.
The audit found that since the Policy for CMP at VAC is relatively new, the program area’s focus has been on setting up the reimbursement process and fine tuning the business rules with the third-party provider. Similar to other entitlement-based treatment benefits, the management focus has been on eligibility and access. The program area has collected and monitored some data, however, trend analysis on health and well-being of the Veteran has not been the priority. There is regular reporting from the third party service provider, but it is more transactional and volume-based reporting.
VAC does require some information to be input into the claims system from both the authorization (authorizer name, grams authorized, federal license seller) and the invoice (grams reimbursed, benefit code of product); however, there is opportunity to improve data collection efforts such that key information is captured, logged in the system, and used for policy decisions. We noted that during our field work, VAC was working on a pilot project with one of the federal licensed sellers to implement an electronic billing process in an effort to reduce transactional costs. It was pointed out that VAC intended to use this opportunity to gather additional information by having a dedicated field for the level of THC content of the product being purchased by the Veteran, and to ensure both the authorizer and specialist information are both collected.
Recommendation #4:
It is recommended that the Assistant Deputy Minister of Service Delivery in consultation with the Assistant Deputy Minister Strategic Policy and Commemoration and the Assistant Deputy Minister of Chief Financial Officer and Corporate Services, develop a strategy for the collection and analyses of important data (including but not limited to: conditions treated, cannabis type, CBD/THC, methods of administration, etc.) to inform policy and a monitoring framework.
Management agrees with this recommendation.
Service Delivery and Program Management is committed to collaborating with the Policy and Research Division, the Health Professionals Division, the Access to Information and Privacy Division, and the Statistics Division, to develop a strategy for the proper collection and analysis of additional data to inform both policy and a monitoring framework within the Department’s authority.
3.4 Monitoring usage trends
VAC does not monitor trends in usage of CMP.
Without collecting and analyzing critical information about Veterans’ use of CMP, the department cannot identify trends that may be problematic and adjust policy to safeguard the health and well-being of Veterans.
VAC’s mandate, the treatment benefits performance indicators, and the Reimbursement Policy on Cannabis for Medical Purposes (the Policy) all have objectives centered around Veteran health. Given this objective and the lack of research and evidence supporting the efficacy and safety of CMP, we expected VAC to monitor CMP usage trends and take action where warranted. We expected VAC to monitor things such as:
- significant increases in dosages;
- links to conditions that medical organizations characterize as “contraindications;” and
- high CMP use coupled with problematic drug groups.
We found that VAC did not monitor these trends in usage. Most people we spoke to at the Department stated that VAC should be doing more in this regard; however, no action has yet been taken. We also spoke to one independent insurance company who advised that they do monitor drug usage for specific types of drugs and take action when amounts exceed recommended rates. They regularly contact pharmacies and physicians when problems are identified.
One recommendation from The College of Family Physicians of Canada (CFPC) in their guidance for authorizing CMP is that “until further research clarifies effectiveness/harms in treating anxiety, PTSD, or insomnia, cannabis is not an appropriate therapy for these conditions.”
However, they did note that when a physician decides to authorize cannabis treatment for patients with co-existing anxiety and neuropathic pain, it is recommended that they:
- keep the dose low to avoid triggering anxiety;
- considers indicating low THC content or CBD-only strains on the medical document; and
- discontinue cannabis if the patient’s anxiety or mood worsens.
Further, the CFPC notes that physicians should consider tapering patients on high doses of opioids or benzodiazepines.Footnote 21
Health Canada has also cautioned physicians to use extra care when considering authorizing CMP to patients with:
- respiratory diseases such as asthma or COPD;
- a history of substance abuse; and
- mood disorders or who are taking sedatives or other psychoactive drugs
Given that VAC had not done any analyses on these higher risk situations, the audit team conducted its own analyses on contraindications of disability benefit entitled conditions and drug usage. The audit team analyzed information on all the Veterans being reimbursed for CMP during our scope period and found that:
- the vast majority have mental health conditions, in particular Post Traumatic Stress Disorder (PTSD), which are considered a contraindication by health organizations such as the College of Family Physicians of Canada and Health Canada; and
- 45 Veterans whose entitled condition is for a substance abuse disorder.
- 46 Veterans had been reimbursed for a high amount of CMP (7-10 grams/day) and had also been reimbursed for all four categories of high-risk drugs: anti-depressants, anti-psychotics, Benzodiazepines, and opioid/narcotics.
- In addition to those 46 Veterans, 149 Veterans had been reimbursed for a high amount of CMP (7-10 g/day) and had also been reimbursed for three of the four categories of high-risk drugs.
VAC does have a policy entitled Prescription Drugs (POC 10) where it describes its adverse drug utilization evaluation (ADUE) process, stating “The Department can impose quantity limits on a case-by-case basis where a client's use of POC 10 benefits is deemed possibly to be excessive, including situations of adverse drug utilization.”
Further information on VAC’s website indicates that the ADUE may result in several actions including education of the client on the ramifications of inter-drug relationships, consultation with the physician, consultation with the pharmacist, and referral of suspected breach of ethics or malpractice by a physician.
The audit team was advised that CMP was excluded from ADUE process because it is technically not an approved regulated drug. We were further advised that VAC was undergoing changes to its ADUE process to look at global trends rather than at the individual Veteran level.
3.5 Monitoring Authorizers
VAC does not monitor trends in CMP authorizers.
With limited guidance available on authorizing CMP, there is a risk that some health care practitioners may be over-prescribing the treatment.
CMP is authorized by the number of grams per day, not prescribed like drugs which have standardized dosages. Medical professionals essentially are the gatekeepers for patients seeking to access CMP in Canada. Federal laws allow authorizers to be physicians or nurse practitioners. VAC has outlined an additional requirement for those Veterans seeking reimbursement under the exceptional process (i.e., greater than 3 grams/day). In these cases, a physician with a specialty in the particular medical diagnoses (for example chronic pain, mental health, etc.) must recommend/endorse the request.
Given the potential risk to Veteran health and well-being, we expected VAC would monitor trends in CMP authorizers and take action where warranted. We found that VAC did not monitor trends in CMP authorizers. The audit did note that other organizations operating in an insurance payer model did not take the same hands-off approach. Rather, these organizations conducted data analyses on physician transactions to identify outliers and took actions where warranted.
Since VAC did not monitor these trends, the audit team conducted its own analyses. In its attempts, the team noted serious data integrity issues with the authorizer data that made it impossible to know the full picture. Specifically:
- For roughly one third of the Veterans authorized during our scope, the authorizer field was blank. The third party service provider indicated that these would be instances of nurse practitioner authorizations; however, information from our file review showed this was not always the case.
- The authorizer field, when populated, had data integrity issues where there were multiple instances where the same physician was listed multiple times, with multiple id numbers, and with variations on spelling.
- The authorizer field, when populated, was used inconsistently. In some cases, it was the authorizing physician and in other cases, it was the specialist physician.
Even though we were unable to determine the complete profile of the physician authorizer’s activities, there were some concerning trends. Removing the blank providers from the calculation, the audit noted:
- Eleven authorizers accounted for almost 40% of the Veterans authorized for CMP.
- Five authorizers accounted for just over 1/4, and these authorizers all authorized high average daily dosages as well.
- Only a small proportion (6.5%) of authorizers were authorizing for more than 3 grams/day.
Recommendation #5:
It is recommended that the Assistant Deputy Minister of Service Delivery develop a risk-based monitoring framework for CMP use with a lens for the health and well-being of Veterans. The framework would support the data strategy (noted in recommendation #4) and include:
- monitoring such things as increased usage, links to conditions being treated, mental health conditions, other drugs being used, contraindications, cannabis type and method of administration, as well as CBD and THC strengths.
- criteria that would identify Veterans that are at high risk and ensure they have the appropriate supports available (i.e., Case management, additional treatment benefits, substance abuse supports, Operational Stress Injury clinics).
- criteria for monitoring authorizations and escalating trends of over-prescribing CMP to the appropriate provincial medical regulatory bodies (i.e., college of physicians) for their own investigation.
Management agrees with this recommendation.
Service Delivery and Program Management will develop a risk-based monitoring framework for CMP use with a lens for the health and well-being of Veterans.
Consultations will be held with the Health Professionals Division, the Access to Information and Privacy Division, Information Technology, Legal Services and the Policy and Research Division to develop a monitoring framework within our authority to identify Veterans at risk and develop a strategy to address those at risk.
3.6 Daily authorized limits
Veterans are not being reimbursed for more cannabis than for which they were authorized.
An authorizing health care practitioner will indicate on the medical document the amount of grams/day being authorized. We expected that VAC would have controls in place to limit reimbursements to the amount of cannabis that had been authorized. Our file testing found that the process is manual in nature and complicated with various dates; however even with these elevated risk factors, Veterans were not being reimbursed for more cannabis than for which they were authorized.
3.7 Monitoring spending
Program Spending:
Spending on CMP is increasing at a significant rate. While the department did see a temporary decrease in spending after the implementation of the Reimbursement Policy for Cannabis for Medical Purposes in November 2016, demand for CMP continues to grow.
The Prescription Drug Program (also known as POC 10) is one of 14 treatment benefit programs, or Programs of Choice (POC), offered by VAC to eligible clients. POC 10 provides drug products and other pharmaceutical benefits to eligible clients who have:
- a demonstrated medical need and;
- health professional authorized to prescribe pharmaceuticals
As shown in Figure 5, VAC now spends more on CMP than it does for all prescription drugs combined.
Figure 5 : CMP vs Other Prescriptions
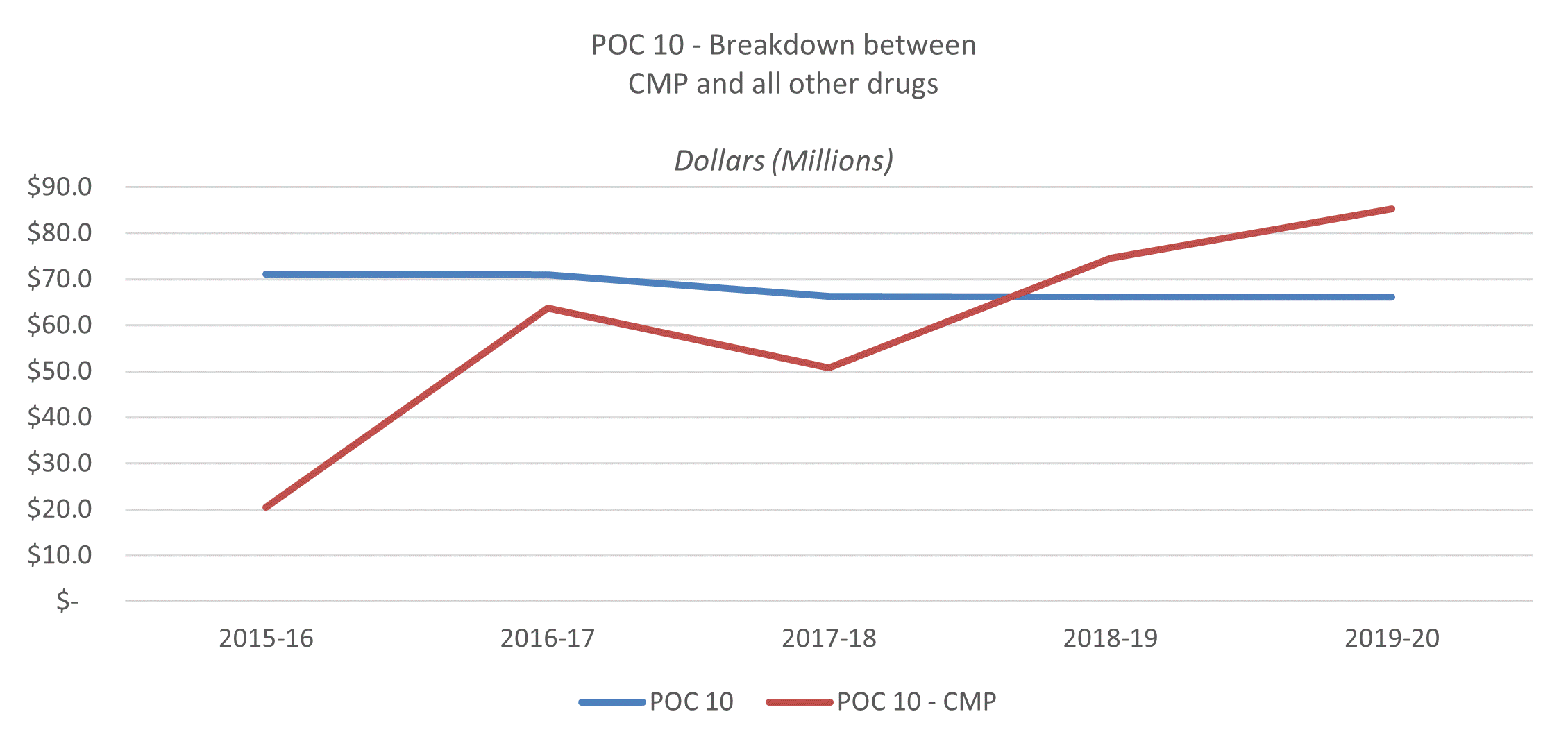
Figure 5 : CMP vs Other Prescriptions
| POC | 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 |
|---|---|---|---|---|---|
| POC 10 | $71.1 | $70.9 | $66.3 | $66.2 | $66.1 |
| POC 10 - CMP | $20.5 | $63.7 | $50.8 | $74.6 | $85.2 |
Given the significant growth, the audit team expected VAC would monitor CMP spending. We found that VAC had monitored and forecasted spending on CMP primarily through its annual budgeting exercise which is conducted by VAC finance.
The process is systematic and robust and finance staff consult with program area as needed. However, VAC flat-lined its CMP projections in its most recently available Facts and Figures publication. This meant that VAC showed actual 2019-20 CMP spending at $85.2 million and forecasted CMP spending at $143.6 million for each of the 5 next fiscal years. VAC does not flat-line other forecasts. Departmental staff advised that they did not forecast out like other programs because it was relatively new and hard to predict.
Upon discussion with the audit team, VAC staff agreed that sufficient time had passed to formulate projections for CMP spending. At the time of writing, new projections were as shown in Figure 6.
| 2020-21 | 2021-22 | 2022-23 | 2023-24 | 2024-25 | 2025-26 |
|---|---|---|---|---|---|
| $119.0 | $156.0 | $195.2 | $233.9 | $276.0 | $321.5 |
Transactional spending:
In addition to program costs (i.e. the cost of the cannabis itself), there are also transactional costs paid to the 3rd party service provider to process authorization requests and invoice payments. These fees are outlined in the contract terms and conditions. The contract is managed by VAC’s Contracting Administration Unit. We found that VAC’s Contracting Administration Unit, in consultation with the program area, had monitored and forecasted spending related to the transactional costs associated with CMP processing (FHCPS contract). Transactional costs are high and VAC’s Contracting Administration Unit has forecasted these costs to rise to $1 million per month by 2026.
3.8 Maximizing Value of Public Funds
VAC has recognized the growth in demand for CMP but could implement more measures to maximize value of public funds.
Program spending:
Given the historical growth in cannabis spending coupled with the projected continued growth in spending, we expected VAC would have recognized the growth and devised mitigation strategies to address value for cost (e.g., industry partnerships, generic options etc.). We found that VAC had recognized the growth in CMP program spending but had not taken action to identify solutions that would maximize the value of funding for the program.
Reimbursement for CMP falls under treatment benefits which is one of the twenty-five separate quasi-statutory programs managed by VAC. This quasi-statutory funding is demand driven and non-discretionary. In essence, if a Veteran is eligible to use CMP VAC must reimburse the Veteran for the amount and price that fall within the policy.
VAC Finance is monitoring the expenditures monthly as is required under the Treasury Board Financial Management Policy to ensure the sound and prudent use of public funds and accountability to Canadians.
Transactional spending:
VAC’s Contracting Administration Unit had recognized the growth in CMP transactional spending and had identified various options to attempt to reduce these costs. VAC’s Contracting Administration Unit has a planned pilot project with one of the Federal Licensed Sellers to operationalize one of these cost mitigating options.
Recommendation #6:
It is recommended that the Assistant Deputy Minister of Service Delivery in consultation with the Assistant Deputy Minister of Chief Financial Officer and Corporate Services implement cost-effective solutions related to administrative or product costs.
Management agrees with this recommendation.
Service Delivery and Program Management is committed to consult with Finance Division to seek out ways to identify cost-effective ways to manage the growth of the program.
3.9 Reimbursement rate per gram
VACs Reimbursement Policy for Cannabis for Medical Purposes (the Policy) states that it will reimburse Veterans based on a maximum rate per gram. The policy does not outline the maximum rate, but at the time the policy was established in 2016, the rate was set at $8.50/gram of dried cannabis (or its equivalent in other forms) based on market research at the time.
We expected that VAC would have actively monitored the reasonableness and relevancy of the $8.50/gram reimbursement rate. We found that VAC has been unable to conduct the necessary market research to ascertain whether the $8.50 rate remained appropriate. Federal License Sellers no longer report their prices publicly on their websites, and as such, VAC has not been able to access the market comparables.
Since completing the audit fieldwork, VAC was able to assess and validate the daily reimbursement rate through the third-party service provider that manages the CMP claims.
3.10 Audit Opinion
VAC has taken steps to operationalize its policy to provide Veterans with access to reimbursement for their CMP treatment. However, there remain serious gaps in internal controls in the areas of Veteran health and program management.
As Health Canada has not approved CMP as a therapeutic treatment, VAC must take considerate and cautious measures in improving oversight when supporting Veterans in this treatment through the reimbursement of costs. VAC has an opportunity to consult stakeholders and engage with health experts in further developing a stronger policy and monitoring framework within our authority that will support the health needs of Veterans and their families.