ISBN: 978-0-660-78629-2
Download full report
PDF Version
Table of Contents
- Executive summary
- Glossary of terms
- 1.0 Introduction
- 2.0 Scope and Methodology
- 3.0 Relevance
- 4.0 Effectiveness, efficiency and economy
- Conclusion
- Recommendations
- Appendix A: Status update on the 2022 Office of the Auditor General’s Processing Disability Benefits for Veterans audit report recommendations
- Appendix B – Service standards of other government departments
Executive summary
Veterans Affairs Canada's (VAC's) mandate is to support the well-being of Veterans and their families, and to promote recognition and remembrance of the achievements and sacrifices of those who served Canada in times of war, military conflict and peace. One way VAC accomplishes this is by providing compensation to Veterans in recognition of disabilities related to their military service, or that have been aggravated by their service. There are a suite of disability benefits available, with the main benefits being Pain and Suffering Compensation (PSC) and Disability Pensions (DP). VAC delivers the suite of benefits through the Disability Benefits (DB) program. The DB program has been VAC's signature program for many decades, and is often the program for which Veterans first apply for benefits from the department. PSC is the most recent evolution of the compensation offered that provides recognition to Veterans and serving CAF for permanent service-related disabilities
This evaluation focused primarily on PSC, which was implemented in April 2019 as part of the Pension for Life (PFL)Footnote 1 initiative that further supports Veterans, serving Canadian Armed Forces members and their families. The evaluation examined the relevance and performance of PSC and was conducted in accordance with Treasury Board Secretariat (TBS) Policy on Results requirements. While the evaluation is focused on PSC, the report contains information on the overarching DB program for contextual purposes as there is significant overlap in the delivery of, and reporting on, PSC and DP.
The PSC benefit is a non-taxable monetary benefit that recognizes and compensates for the non-economic effects of service related disabilities. When a Veteran receives a favourable decision, the benefit is automatically paid as a monthly amount for life, unless the Veteran chooses to cash out the value and take the amount as a lump sum payment. As of 1 April 2024 PSC monthly payments range from $67.77 to $1,355.38 for the life-time monthly amount or from $22,049.60 to $440,991.96 as a lump sum, and approximately 36% of Veterans chose to receive the monthly amount.
In order to be considered for a PSC benefit, an application form must be completed that provides details of the applicant's disability and service. An applicant must have a diagnosis of a medical condition or disability and be able to show that the condition or disability is related to service or has been aggravated by service. Additionally, medical information from health care professionals is often required to support the application.
Once all of the necessary information is obtained the application is forwarded to a trained decision-maker that specializes in disability benefits decisions. The decision-maker independently examines the evidence the applicant submitted as well as the information obtained by VAC on behalf of the applicant and applies relevant legislation, policies and guidelines in making decisions.
The main service standard for the DB program is that 80% of first applications will be completed within 16 weeks of an application that has all of the necessary information to render a decision. The number of applications taking longer than 16 weeks to be completed had been increasing between 2015 and 2020 due to the increasing number of applications being received by VAC and the increased complexity of some applications. VAC received temporary funds in 2020 to help address the high number of applications awaiting processing. The funding was renewed in 2022 and 2024, and has resulted in significant progress in adjudicating more applications and to better meet the service standard, with 76% of first applications completed within 16 weeks during the fiscal year 2023-24.
The evaluation team found that there is a continued need and an ongoing high-level of demand for compensation through PSC. Over the past several years, the number of annual applications received has continued to increase, and VAC has responded by completing more applications, resulting in more Veterans receiving their compensation and recognition.
The PSC aligns with government priorities and federal government roles and responsibilities: providing benefits and services is the responsibility of the federal government and VAC is the department mandated to fulfill this responsibility.
A number of initiatives have been implemented or were in-progress over the scope of the evaluation to enhance the effectiveness and efficiency of the DB program. There is performance information available to support the evaluation; however, targets have not been reached, with segments of the Veteran population reporting much lower rates of feeling compensated and recognized through their PSC benefit. One of the ultimate outcomes is not an appropriate measure of the PSC benefit, and there is significant overlap in the intermediate outcomes for the DB program and PSC benefit yet targets are different.
There are various types of applications (first applications, reassessment and departmental reviews) that VAC receives, with some being straightforward to process and some being very complex. Based on the type of application, the amount of effort required to render a decision varies. New service standards are needed to both reflect time approximate amount of time it will take to complete applications and better communicate with Veterans how long they can reasonably expect to wait for a decision.
Veterans face challenges in obtaining required information to meet the application requirements in a timely manner from an overwhelmed Canadian health care system. While some measures have been taken by VAC to help ease this burden, a further review of application requirements and processes that considers the challenges Veterans, health care providers and departmental employees face in delivering the PSC program would be timely. The complexities should be better communicated to Veterans, and better reflected in the service standards.
There remains significant challenges related to the IT systems employees use to process applications. The goal of having a new system to replace the legacy system that can process all applications has yet to be realized. This has impacts on Veterans, and employees who must work in two separate systems, with workarounds needed in order to process applications, resulting in extra resources and time to process applications.
The addition of multiple rounds of temporary funding has helped get Veterans their decisions in a more timely manner. The department is processing thousands of more applications per year than it was five years ago, and payments to Veterans are higher than at any point in the department's history. In order to maintain this momentum, VAC should continue to find greater efficiencies through more stream-lined processes and IT modernization. With these adjustments, and a formalized forecast of demand, the Department could then more effectively assess the amount of long-term funding needed to ensure applications are processed efficiently, with modernized processes, and in a timely manner.
Recommendation 1:
It is recommended that the Assistant Deputy Minister, Service Delivery, in collaboration with the Assistant Deputy Minister, Chief Financial Officer and Corporate Services develop a Disability Benefits strategy that will enhance the efficiency and experience of the program for both Veterans and employees and build program sustainability. A corresponding action plan will include actions that:
- Streamline workflows and business processes.
- Review and update process requirements, as appropriate, with consideration of the administrative burden on clients, employees, and the Canadian Health Care system.
- Enhance processing through an innovative technology solution that can address disability benefit applications from intake to payment through a single window interface for users.
Recommendation 2:
In conjunction with Recommendation 1, to ensure smaller scale pressures on the disability benefits program are addressed, it is recommended that:
- The Director General Centralized Operations Division, in collaboration with the Director General, Service Delivery and Program Management and the Director General, Information Technology, Information Management, Access to Information and Privacy (ITIMAP), ensure system related process improvements are identified, communicated, and prioritized to support efficient delivery of disability benefits.
- The Director General, Centralized Operations Division continue to invest in adjudicator training and monitoring of medical advisory requests with a view to ensuring only necessary conditions are sent for a medical consult.
- The Director General, Health Professionals Division ensures that the appropriate processes and resources are available to both reduce the current number of applications awaiting a consult, and provide a timely response to future medical consult requests.
Recommendation 3:
It is recommended that the Director General, Centralized Operations Division, in consultation with the Director General, Strategic Planning, Results and Cabinet Business, develop transparent Veteran-focused service standards with consideration of the different types of applications and adjudicative processes.
Recommendation 4:
- It is recommended that the Director General, Centralized Operations Division, in consultation with the Director General Strategic Planning, Results and Cabinet Business review outcomes, results and targets with a view to ensuring they are aligned with the objective of the program and are achievable.
- It is recommended that the Director General, Policy and Research determine why outcome achievement is significantly less for segments of the client population.
Glossary of Terms
The evaluation uses a number of different program specific terms to explain how work is currently being performed within VAC. To support the reader, a glossary of terms has been developed to provide the reader with context.
Application: The formal submission of a request or claim for benefits or services.
Complete Application: An application that includes all required information to allow for an adjudication decision.
Completed Application: An application that has been adjudicated with the Veteran receiving either a favourable decision with the payment amount verified, or an unfavourable decision.
Complex Application: Refers to applications that require review by an employee with a medical background (i.e, a nurse and sometimes a doctor).
Condition: Refers to a single medical condition affecting a Veteran, for which they are applying for a disability benefit.
Departmental Review: Occurs when an applicant has new evidence that was not submitted in their application. A VAC adjudicator reviews the submission, including any new evidence, to determine if a new decision should be issued.
Disability Benefits (DB): A disability benefit is a tax-free, financial payment to support Veterans well-being. There are currently two types of disability benefits: the disability pension and pain and suffering compensation.
Disability Pension (DP): A regular payment to Veterans with disabilities resulting from their military service. This was the initial form of disability compensation for Veterans and is still provided to War Service Veterans and Royal Canadian Mounted Police, and to some CAF Veterans who applied before 1 April 2006.
Disability Awards (DA): Lump-sum payments given to Veterans for specific disabilities or injuries. This was the second iteration of disability compensation for CAF Veterans which started 1 April 2006. This was replaced 1 April 2019 by Pain and Suffering Compensation.
Pain and Suffering Compensation (PSC): Recognizes and compensates serving CAF members and Veterans for the pain and suffering experienced as a result of his or her service-related disability. This is the third iteration of disability compensation for Veterans which started on 1 April 2019.
First Application: The initial submission of a claim or request for benefits for a medical condition.
Incomplete Application: An application that lacks necessary information or documentation to be adjudicated.
In Progress Application: Indicates that the application is being actively reviewed and processed by VAC.
On Hold/Withdrawn Application (e.g., incomplete after 60 days): An application that has been put on hold or withdrawn due to incomplete documentation or other reasons, often due to documentation not being received within 60 days of the Veteran being notified.
Received Application: Confirmation that the application has been received.
Reassessment: The process of Veterans asking the department to review and evaluate a previously approved medical condition due to a change or worsening of a medical condition.
Service Standard: The expected timeframe within which an application should be processed or a service delivered. Currently, the service standard for first applications is 16 weeks, with a target to achieve this 80% of the time.
Service Standard Start Date (SSSD): the date that the department has received a complete application form and all required supporting documentation from the Veteran.
Straightforward Application: Applications containing medical conditions which can be processed by employees without a medical background.
Withdrawn Application - Internal Processing (System Transfer): When VAC transfers an application from one processing system (GCcase) to another (CSDN) due to limitations in GCcase.
Introduction
Veterans Affairs Canada's (VAC's) mandate is to support the well-being of Veterans and their families, and to promote recognition and remembrance of the achievements and sacrifices of those who served Canada in times of war, military conflict and peace. One way VAC accomplishes this is by providing compensation to Veterans in recognition of disabilities related to their military service, or that have been aggravated by their service. There are a suite of disability benefits available, with the main benefits being Pain and Suffering Compensation (PSC) and Disability Pensions (DP). VAC delivers the suite of benefits through the Disability Benefits (DB) program. For the purposes of this report when DB is referenced, it refers to PSC and DP only.
This evaluation focuses primarily on PSC, which was implemented in April 2019 as part of the Pension for Life (PFL)Footnote 2 initiative to further support Veterans, serving Canadian Armed Forces (CAF) members and their families. The evaluation examined the relevance and performance of PSC and was conducted in accordance with Treasury Board Secretariat (TBS) Policy on Results requirements and guidance material. While the evaluation is focused on PSC, the report contains information on the overarching DB program for contextual purposes as there is significant overlap in the delivery of, and reporting on, PSC and DP.
1.1 Pain and Suffering Compensation
When PSC was implemented, it replaced the Disability AwardFootnote 3 as the benefit to recognize and compensate Canadian Armed Forces members and Veterans for service-related disabilities. The PSC benefit is non-taxable and is intended to compensate for pain and suffering. The benefit is automatically paid as a monthly amount for life, unless the Veteran chooses to cash out the value and take the amount as a lump sum payment. As of 1 April 2024 PSC monthly payments range from $67.77 to $1,355.38 for the life-time monthly amount or from $22,049.60 to $440,991.96 as a lump sum.
The number of PSC clients and expenditures have increased since its inception in 2019. Table 1 depicts clients and expenditures, from 2019-20 to 2023-24.
Table 1: PSC Clients and expenditures
| Actual expenditures and clients | |||||
|---|---|---|---|---|---|
| 2019-20 | 2020-21 | 2021-22 | 2022-23 | 2023-24 | |
| Pain and Suffering Compensation ($billions) | $0.92 | $1.09 | $1.54 | $1.39 | $1.61 |
| Unique PSC Payment Clients | 19,050 | 26,175 | 35,934 | 37,672 | 41,865 |
Source: VAC Statistics Directorate
Between 2019-20 and 2023-24 the number of unique payment clients more than doubled, while expenditures grew by a lesser rate. This is due to clients who choose the monthly amount being counted in multiple years, while clients who chose a lump sum amount were only counted in the year they received the payment. The expenditures total for a given year are impacted by the number of application decisions and the choice of payment methodFootnote 4.
1.2 PSC eligibility
To qualify for PSC, you must be a CAF member or Veteran with service after 1 April 1947 (excludes Korean War service), have a diagnosed medical condition or disability, and show that the condition is related to service or has been aggravated by service.
1.3 PSC as part of the Disability Benefits program
VAC delivers disability benefits to Veterans through its Disability Benefits (DB) program. PSC and DP each provide financial compensation in recognition of service-related disabilities. The decision-making process is mostly the same for PSC and DP, including business processes, tools and supports, employees and systems. The main difference relates to the Veteran's service, as this determines whether they qualify for PSC or a DP (War Service Veterans and RCMP qualify for DPs)Footnote 5.
PSC and DP serve as key gateways to accessing many of the benefits and services offered by VAC, including health care benefits, home care and long-term care. Additionally, the DB program comprises several smaller benefits that recognize and compensate qualifying Veterans, serving CAF members, survivors, dependents, RCMP and certain civilians for the effects of a service-related disability and/or death. Depending on the Veterans' service and date of application they may qualify for other benefits from VAC.
1.4 Overview of the application submission and adjudication process
In order to be considered for a PSC benefit, an application form must be completed that provides details of the applicant's disability and service. An applicant must have a diagnosis of a medical condition or disability and be able to show that the condition or disability is related to service or has been aggravated by service. Veterans can submit applications to VAC multiple ways:
- Electronically via My VAC Account (MVA)
- By completing a paper copy of the application form and mailing it or dropping it off to a VAC or Service Canada office
- Through a representative of the Royal Canadian Legion
- Additionally, medical information from health care professionals is often required to support the application.
VAC employees will review the application to determine if all necessary information has been submitted. If anything is missing, an employee will contact the applicant and await the missing information (for more information on incomplete applications see section 4.2.4). VAC will obtain a copy of the applicant's service health records to review in support of the application.
Once all of the necessary information is obtained the application is forwarded to a trained decision-maker that specializes in disability benefits decisions. The decision-maker independently examines the evidence the applicant submitted as well as the information obtained by VAC on behalf of the applicant and applies relevant legislation, policies and guidelines in making decisions. There are a number of aspects that go into making a decision such as establishing the linkage between service and disability, qualifying service periods, and medical diagnosis.
There are two components to the adjudication process for PSC: entitlement and assessment. The level of entitlement is based on the degree to which the disability is related to the Veteran's service. The assessment is based on the extent (level of impairment) of the disability and the impact on the Veteran's quality of life. The disability assessment rating is applied to each condition separately that a Veteran applies for. The combination of these factors will determine the amount of compensation the Veteran receivesFootnote 6. Once the decision-maker makes a decision on the application, a letter will be mailed to the applicant informing them of the decision (the letter will also be made available on MVA for Veterans who use that service). The letter outlines the reason for decision, any compensation the Veteran will receive, and their appeal rights.
1.5 Application types at VAC and service standards
There are three main types of PSC application decisions made by VAC:
- First application: The Veteran's first time applying to VAC for that specific medical condition.
- Reassessment: Veterans can request to be reassessed if the disability for which they are receiving benefits worsens and medical evidence can support that there has been a change in the condition. If it is confirmed that the condition has worsened, the disability benefit is adjusted accordingly.
- Departmental Review: Veterans submit new evidence for consideration that was not included in their original application. Departmental Reviews can be initiated directly by the Veteran or by the Department when there has been an error.
Each of these three application types has its own service standard. The service standard tells the Veteran how long they can expect it will take VAC to make a decision. VAC publishes its performance against many of its service standards on the external departmental website. The current service standard for Disability Benefits is for 80%Footnote 7 of decisions to be made within 16 weeks for first applications and reassessments, and 12 weeks for departmental reviews (see section 4.1: Achievement of expected outcomes for more details on results against service standards, and section 4.2.3 Service standards).
VAC's service standard for first applications is measured as the time from which a complete application is received by the Department to the date the payment amount is verified (for favourable decisions), or the decision date for unfavourable applications. Applications that are ready to be adjudicated or are in the process of being adjudicated but are taking longer than 16 weeks (12 weeks for Departmental Reviews) are deemed to be outside the service standard. As outlined in section 3.1, the number of applications taking longer than 16 weeks had been increasing between 2015 and 2020 due to the increasing number of disability benefit applications being received by VAC and the increased complexity of some applications. VAC received temporary funds in 2020 to help address the high number of applications awaiting processing. The funding was renewed in 2022 and 2024, and has resulted in significant progress in adjudicating more applications and to better meet the service standards.
2.0 Scope and methodology
2.1 Evaluation objective and scope
This evaluation was conducted in accordance with VAC's 2022-23 to 2026-27 Departmental Evaluation Plan, which was developed to align with TBS's Policy on Results. The policy stipulates that evaluations of all ongoing programs funded under a grant and contribution vote that have a five-year average expenditure of $5 million per year or more must be evaluated every five years. The policy also indicates that all organizational spending and all programs in the Department's Program Inventory must be considered within departmental evaluation planning based on risk and need.
The past performance of PSC was reviewed along with current activities to determine program relevance, effectiveness, and economy. The evaluation covers the time period from 1 April 2019 to 31 December 2023. When available and applicable, data up to May 2024 was incorporated into the evaluation.
The scope of the evaluation was focused on PSC, however, there is significant overlap between the PSC and the DP, and the two benefits are administered by the same Division using the same processes and systems. Additionally, the Department's data and reporting was mostly at the DB level prior to the evaluation. The evaluation team worked with operational colleagues to get data specific to PSC. Due to limitations in the data, at times the evaluation team was not able to present only PSC data, so the broader DB data was used.
This is the first evaluation of PSC. The most recent evaluation of the DB program was completed in March 2022 and was focused on the Disability Benefits Redress process.
2.2 Evaluation questions
The objective of the evaluation was to assess program relevance, while considering opportunities to improve program effectiveness and efficiency.
Upon completion of an initial review (interviews, document review, and data analysis), evaluation questions were developed to help assess program relevance and program performance. A list of evaluation questions, highlighting the key lines of inquiry, can be found in Table 2 below.
Table 2: Evaluation Questions
| Evaluation Questions |
|---|
| Relevance |
| Performance |
| To what extent is Pain and Suffering Compensation responsive to the needs of Veterans? |
| To what extent does the Pain and Suffering Compensation align with Government of Canada priorities and with federal roles and responsibilities? |
| To what extent is the Pain and Suffering Compensation achieving its intent and contributing to the overall outcomes of the Disability Benefits Program? |
| Are there opportunities to improve the efficiency of the delivery of the Pain and Suffering Compensation? |
2.3 Evaluation methodology
The evaluation was summativeFootnote 8 in nature and relied on a mix of qualitative and quantitative data sources. The methodology incorporated multiple lines of evidence to ensure reliability of collected information and reported results. This information is further outlined in Table 3 below.
Table 3: List of evaluation methodologies and sources
| Methodology | Source |
|---|---|
| Document review | The following departmental documents/information were reviewed to understand the program's objectives/intent, relevant authorities, complexity, context and any key issue areas: planning documents, central agencies documentation, previous audits and evaluations, policies, business processes, guidelines, records of decisions, strategic documents, performance reports, research papers, and survey results. |
| Non-departmental document review | Various non-departmental documents such as: literature from other federal departments. Also, reports from the House of Commons Standing Committee on Veterans affairs (ACVA), Office of the Veterans Ombudsman reports, the federal budget, mandate letters, and speeches from the throne. |
| Data analysis | Client data and program performance data as of December 2023 was analyzed with more up-to-date information taken into consideration where available. Where complete data was available, statistical analysis was conducted to support the findings of the evaluation. |
| Key informant interviews | Over forty interviews were conducted with VAC senior management, program employees, and other relevant subject matter experts. |
| Observation | Observation of systems and application processing was conducted to better understand the application and decision-making process. |
2.4 Considerations and limitations
- The evaluation team did not speak directly with individuals in receipt of PSC. This limitation was partially mitigated by:
- Reviewing existing public opinion research such as the 2020 and 2022 Veteran National Client Surveys and the Let's Talk Veterans platform
- Conducting interviews with VAC employees who work directly with Veterans and PSC applications
- The introduction of the PSC program in 2019 coincided with the release of the GCcase benefit processing system. Before 2019, all Disability Benefits processing took place in the Client Service Delivery Network (CSDN). After 2019, some DB applications were processed in GCcase, while others needed migration to CSDN. This complicates data retrieval and analysis. Pre-published statistics for the DB program were used where available.
- The Department forecasts the number of clients based on available adjudication resources. There is no official forecast of demand for the program; however, the evaluation used an internal forecast prepared for another purpose.
- The evaluation was conducted while improvements to program delivery were underway (e.g., backlog reduction). Impacts of these improvements were considered where possible.
- Due to departmental methodology for tracking operating costs, the evaluation team could not report on the overall administrative budget specific to PSC or estimate program resource utilization costs with confidence. VAC provided historic resource levels for disability benefit decision makers and support staff, which served as a proxy to illustrate resource investment addressing program pressures such as the backlog.
The above noted information should be taken into consideration when reading this evaluation report.
3.0 Relevance
3.1 To what extent is the Pain and Suffering Compensation program responsive to the needs of Veterans?
The implementation of Pension for Life (with Pain and Suffering Compensation a key benefit) was the Department's response to better meet Veterans' needs. The number of applications for PSC have continued to increase, and future demand is estimated to remain at high levels.The implementation of Pension for Life (with Pain and Suffering Compensation a key benefit) was the Department's response to better meet Veterans' needs. The number of applications for PSC have continued to increase, and future demand is estimated to remain at high levels.
3.1.1 Being responsive to requests from Veterans
Shortly after the introduction of the Disability Award as part of the New Veterans Charter in 2006, Veteran stakeholder groups began asking the government to return to a monthly pension. In 2011, the Government of Canada responded and made enhancements to the New Veterans Charter, including the Disability AwardFootnote 9. Veteran stakeholder groups continued to call for a return to a monthly pension. In 2018, the Government of Canada announced the Pension for Life initiativeFootnote 10 (the new benefits were implemented 1 April 2019). The PSC was a key component of PFL and was developed to provide Veterans with a choice on how they would like to receive each awarded amount. The monthly amount is the default payment method; however, Veterans may contact the Department and elect to cash out any remaining balance. These changes demonstrate how VAC recognizes and compensates Veterans has continued to evolve to better meet needs and align with the Government of Canada direction.
When designing the PSC, an actuarial analysis estimated that 57% of Veterans would choose the lifetime monthly amountFootnote 11. The results of the actuarial forecast conducted for the Department presumed that Veterans up to a certain age (males aged 56 or younger, and females aged 59 or younger) would choose the monthly option as it could result in the largest lifetime financial benefit. Veterans are eligible to be reimbursed for up to $500 for financial counselling to help determine the best option based on their individual circumstances. The actuarial forecast did not factor in other options Veterans may consider such as taking a lump sum and investing it, putting it towards personal purchases or other reasons. Between 1 April 2019 and 31 March 2023 only 36% of Veterans who received a favourable PSC decision kept the monthly benefit whereas 64% chose to cash-out and receive a lump sum payment, not aligning with original expectations that Veterans wish to receive a monthly pension. The evaluation team did not examine the reasons behind Veterans' financial decisions. However, from a program design perspective, the intent to provide Veterans with a lifetime monthly benefit is not being met to the extent expected. Having the majority of Veterans choose the lump sum amount requires additional administration by the Veteran and the Department as the Veteran needs to contact VAC and complete a form to cash out any remaining value. VAC needs to then process this change in payment. Note: Prior to the end of evaluation's fieldwork VAC has begun including the cash-out forms with favourable decision letters, which will save a step for Veterans who want to cash-out the value of their PSC benefit.
3.1.2 Being responsive to the increased demand for Disability Benefits
From 2015-16 to 2023-24, annual DB applications (including for PSC) received by VAC increased 78%. Table 4 below depicts the number of DB applications received since 2010. The data shows there was a declining trend in DB applications from 2010-11 to 2014-15, before increasing in 2015-16 and each year since, except for 2020-21 which is attributable to disruptions due to the Covid-19 pandemic.
Table 4: Historical DB applications have been rising in recent years
| Fiscal Year | Applications Received - Disability Benefits |
|---|---|
| 2010-11 | 43,731 |
| 2011-12 | 40,197 |
| 2012-13 | 38,766 |
| 2013-14 | 37,564 |
| 2014-15 | 37,502 |
| 2015-16 | 44,986 |
| 2016-17 | 45,368 |
| 2017-18 | 52,297 |
| 2018-19 | 60,975 |
| 2019-20 | 62,892 |
| 2020-21 | 45,500 |
| 2021-22 | 66,255 |
| 2022-23 | 72,575 |
| 2023-24 | 80,256 |
The increases in applications for the DB program (including PSC applications from 2019) resulted in a backlog of applications (i.e, applications waiting to be processed that are outside the service standard). VAC's processing capability was unable to match the increase in applications and this resulted in over 22,000 applications in a backlog as of 31 March 2020. To address the backlog, the Department hired hundreds of new employees and undertook a number of initiatives, as outlined in a strategic direction document on the Department's website.
Approximately 350 new employees were hired on a temporary basis for the fiscal years 2020-2021 and 2021-2022. Most of these employees were dedicated to adjudicating applications, which resulted in a significant reduction in the number of applications outside of the service standard. As of 28 June 2024, there were 5,177 DB applications waiting to be processed that were outside the service standard, which is a significant improvement over the 22,138 that existed prior to the temporary staffing initiative in early 2020 (see Table 5 below for details).
In terms of the service standard, in 2023-24 76% of PSC first applications (69% of DB) were adjudicated within the 16-week time frame, closer to the target of 80%. Based on an 80% target, VAC is communicating that there will be 20% of applications that will take longer than the 16-week service standard (one reason being the complexity of some applications). For example if VAC adjudicates 50,000 first applications in a year, 10,000 of the 50,000 could be expected to take longer than 16 weeks.
Table 5: Historical DB applications outside of the service standard
| March 31, 2020 | March 31, 2021 | March 31, 2022 | March 31, 2023 | March 31, 2024 | June 28, 2024 | |
|---|---|---|---|---|---|---|
| Applications outside of the service standard (backlog) | 22,138 | 15,214 | 11,619 | 6,621 | 5,637 | 5,177 |
In 2022 VAC received funds to extend the temporary employees until March 2024 in support of further reducing processing times. In November 2023 the government announced that they would again extend funding for these temporary resources for an additional two years (through to March 31, 2026). The Office of the Auditor General of Canada (OAG) in its 2022 Processing Disability Benefits for Veterans report recommended that VAC establish a sustainable long-term resourcing plan for processing disability benefit applications in a timely manner. To date, VAC has only been able to secure government approval for additional temporary resources. See Appendix A for more information.
Another initiative the Department implemented to better respond to Veteran's unmet needs resulting from the backlog was the Mental Health Benefit (MHB) that started in April 2022. This benefit allows Veterans who have applied for a disability benefit for certain mental health conditions to have access to immediate mental health care coverage through the Treatment Benefits Program while they await their disability benefit decision. In 2022-23 10,335 Veterans were granted access to the MHB and 9,189 in 2023-24. Since the MHB benefit was implemented there have been 6,004 Veterans that have made at least one claim for reimbursement of a health care benefit.
In a January 2024 media article, the Minister of Veterans Affairs noted that reducing processing times for Veterans awaiting decisions for the Disability Benefits program was her top priority. VAC provides periodic updates on its website regarding processing times and the number of applications in the backlog. This highlights the importance the Department is placing on improving processing times and being responsive to Veterans' needs.
3.1.3 Demand for PSC
There is strong demand for PSC, which is evidenced by the number of applications received. See Table 6 below for data related to PSC applications received from 2019-20 to 2023-24. This increase in applications supports that PSC is both relevant and needed by Veterans.
Table 6: Overview of PSC applications received
| Fiscal Year | 2019-20 | 2020-21 | 2021-22 | 2022-23 | 2023-24 |
|---|---|---|---|---|---|
| First Application | 36,007 | 25,595 | 38,336 | 41,968 | 46,081 |
| Departmental Review | 2,025 | 776 | 1,632 | 1,514 | 1,886 |
| Reassessment | 7,828 | 6,349 | 7,967 | 10,298 | 10,708 |
| Total | 45,860 | 32,720 | 47,935 | 53,780 | 58,675 |
Source: Disability data set
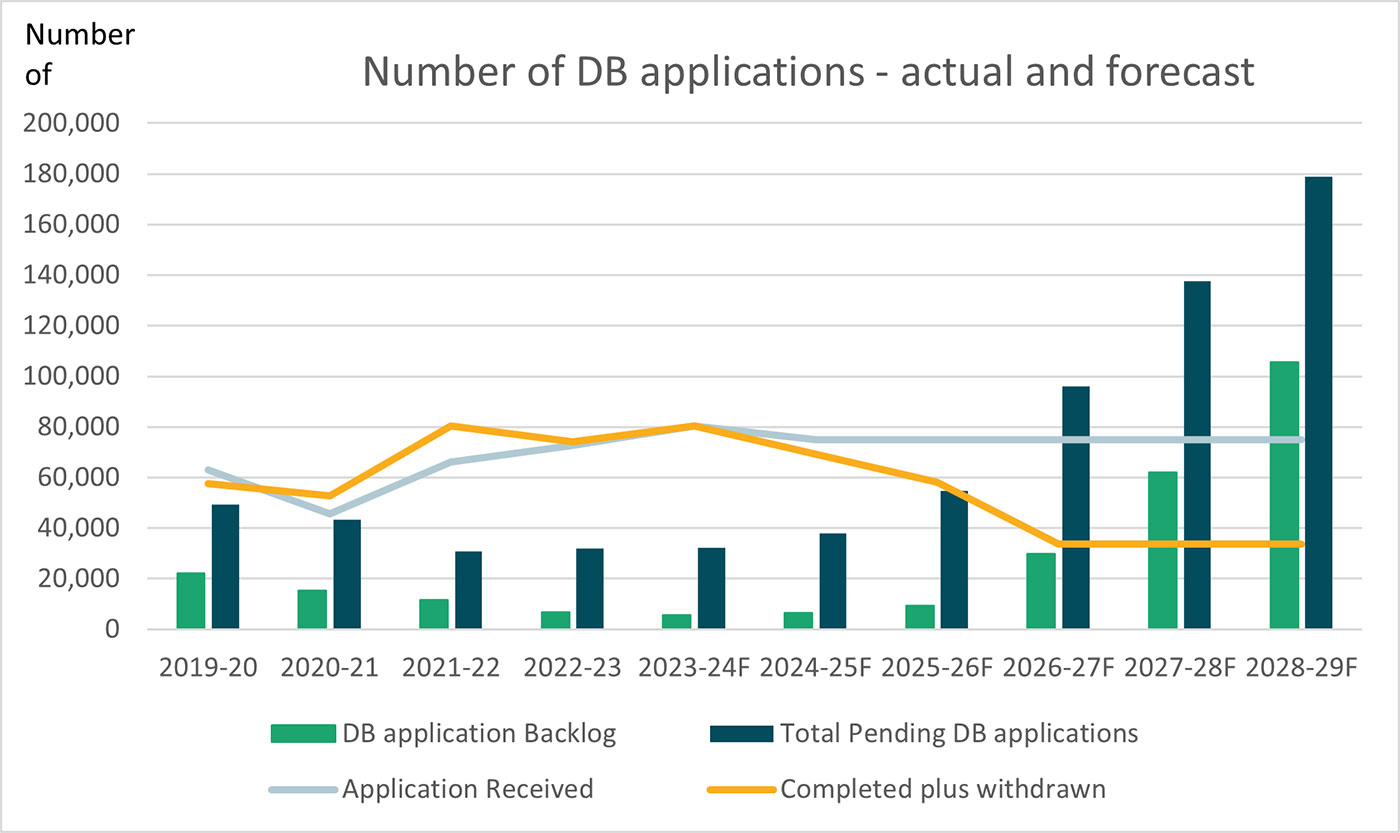
As noted above in section 2.4 Considerations and Limitations, there is no official forecast of demand for PSC; however, the evaluation utilized a forecast for DB that the Department had prepared in support of funding proposals (see Chart 1 below). The forecast shows the demand (applications received) for disability benefits remaining high into the foreseeable future and the need for the program will continue. For fiscal year 2023-24 the Department forecasted it would receive 80,400 DB applications and forecasted an additional 75,000 each year through to 2028-29. With PSC applications being approximately 73% of the total DB applications received throughout the evaluation scope, this equates to a potential estimate of 54,750 PSC application each year from 2023-24 to 2028-29Footnote 12.
Chart 1 below shows the forecasted volumes pertaining to the backlog, pending, completed and withdrawn applications. See section 4.2.4 for more details on the impact of the forecast remaining high and the volume of applications completed and withdrawn decreasing as the temporary funding for additional employees is only until March 31, 2026.
Chart 1: DB applications - actual and forecastedFootnote 13
3.2. To what extent does Pain and Suffering Compensation align with Government of Canada Priorities and with federal roles and responsibilities?
Pain and Suffering Compensation aligns with Government of Canada direction and the mandate of the Department.
The Department's mandate and role is directly tied to the delivery of the PSC benefit, as highlighted in the Department's mandate statement: Veterans Affairs Canada fulfills its mandate and role through the delivery of programs such as disability benefits, financial benefits, health care benefits, rehabilitation, pension advocacy, education, and training supports.
Alignment with Government of Canada direction and departmental roles and responsibilities is also evident through mandate letters to the Minister of Veterans Affairs (2017, 2019 and 2021), and federal budgets (2018 and 2021).
- The government's commitment to improving the DB program is highlighted in mandate letters from 2017, 2019 and 2021.
- The 2017 mandate letter to the Minister of Veterans Affairs tasked the Minister with re-establishing a life-long pension option;
- The 2019 mandate letter references streamlining benefits to reduce overlap and administrative burden; and
The 2021 mandate letter tasked the Minister to continue to reduce wait times and ensure Veterans and their families receive decisions on applications in a timely manner, through investing resources to adjudicate applications, enhanced disability benefit processing and advancing innovative digital solutions.
In addition to the mandate letters, federal budgets have indicated the Government of Canada places a priority on meeting the needs of Veterans. The 2018 Budget stated:
"On 20 December 2017, the Government unveiled its Pension for Life plan, a program designed to reduce the complexity of support programs available to Veterans and their families. It proposes a broader range of benefits, including financial stability, to Canada's Veterans, with a particular focus on supports for Veterans with the most severe disabilities."
Furthermore, the 2021 Budget announced the mental health benefit for Veterans awaiting a disability decision and provided funding to retain temporary employees in support of the efforts to reduce wait times for disability benefits applications.
VAC's responsibility to deliver PSC is outlined in the Veterans Well-being Act, with responsibilities for the Disability Pension (also part of the Disability Benefits Program) outlined in the Pension Act. Priorities in the departmental plans focus on service excellence and enhancements using technology. The 2023-24 departmental plan outlines the importance the Department is placing on reducing wait times for Disability Benefit applications and modernizing through automation and digitization. VAC continues to identify its overarching purpose to support the well-being and recognition of Canada's Veterans, and to provide support to the most vulnerable Veterans.
The evaluation team confirms, primarily through document review, that recognizing and compensating Veterans with PSC supports the Department in meeting its mandate and fulfilling its responsibilities.
4.0 Effectiveness, efficiency and economy
4.1 Achievement of expected outcomes
Pain and Suffering Compensation performance information is being collected and reported on; however, several targets have not been met over the scope period of the evaluation and there is an opportunity to review and enhance targets.
A Performance Information Profile (PIP) identifies the performance information for each program in a department/agency's Program. Each PIP outlines program outputs and outcomes, as well as related performance indicators, targets, data sources and associated methodologies. VAC's Integrated Planning and Performance unit, along with program management employees are responsible for monitoring and overseeing PIPs, while VAC policy officials would have been initially involved in developing the outcomes. Achievement of results are shared with the Department's Performance Measurement and Evaluation Committee (PMEC).
The DB PIP is shared among multiple benefits, including PSC, DP, and other allowances and benefits under the DB umbrella. This evaluation reports on only PSC and DP performance information.
Most of the information presented in the PIP comes from internal data, and the biennial VAC National Client Survey, which was last conducted in 2022. Program results for relevant outputs, outcomes and related indicators were documented for the period of the evaluation. Output and outcome results were reported in the Department's Performance Outcomes and Indicators System. As part of the evaluation, data was analyzed against targets and performance over prior time periods.
4.1.1 Effectiveness
This section contains performance information specific to PSC and also to the overarching DB program. The objective of the program is to compensate Veterans/CAF members and other clients in recognition of the effects of service-related disabilities. Below are some of the key measures the Department uses to help determine the extent the objective is being met.
Immediate Outcome: Veterans receive benefit decisions for Pain and Suffering Compensation in a timely manner.
The Department uses application processing turnaround time as an indicator of success when measuring whether the immediate outcome is being met. The current service standard for PSC processing is 80% of first applications will be processed within 16 weeks. As of 1 April, 2022Footnote 14, the timeframe to measure this indicator begins when the Department receives a complete application with all necessary supporting documents and ends on:
- the date the amount to be paid has been verified; or
- the date an unfavorable decision is rendered.
The target is to make these decisions within 16 weeks 80% of the time. See Table 7a below for results.
Table 7a: Immediate Outcome Performance Measure (PSC)
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| % of Pain and Suffering Compensation first applications for which a decision is made within 16 weeks (Target - 80%) | 23% | 24% | 47% | 61% | 76% |
The Department has significantly improved performance related to meeting this outcome. This is also true for DP (combined with Pain and Suffering Applications). See Table 7b below for results for the Disability Pension/Pain and Suffering Compensation (also referred to as Disability Benefits throughout this report) against the 16-week service standard.
Table 7b: Immediate Outcome Performance Measure (DP and PSC)
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| % of Disability Pension / Pain and Suffering Compensation first applications for which a decision is made within 16 weeks (Target - 80%) | 23% | 30% | 46% | 55% | 69% |
The Department has improved its percentage of claims meeting the 16-week service standard throughout the scope period of the evaluation due to a reduction in processing times. The average processing time for PSC first applications decreased from 41 weeks for the fiscal year 2019-20 to 17 weeks for the period of October to December 2023 (section 3.1 has more details on how the Department achieved this). Processing times for DB first applications decreased from 44 weeks during the period of July to September 2021 to 18 weeks during the period of October 2023 to December 2023.
Although there has been improvement in the percentage of claims meeting the 16-week service standard, Tables 7a and 7b show PSC and DB are not yet meeting the 80% target. There is a single indicator for the immediate outcome decisions made within 16 weeks, and this does not reflect differences in information and time required to process the variety of applications, and the different processing streams that the Department has in place. For example, at VAC a streamlined process is used to render decisions faster for specific health conditions that are more common such as hearing loss, musculoskeletal and post-traumatic stress disorderFootnote 15. Other processes for more complex conditions require additional steps that impact the length of time it can take to reach a decision on an application. For example, VAC may require additional tests or information from doctors and other health professionals, and within the adjudication process, the application may be sent to a medical advisory unit for further review due to the complexity of the medical conditions for which the Veteran applied.
At times, the Department's disability benefits workload appears to have been guided by a desire to meet the 16 week service standard as much as possible, giving priority to applications that could be adjudicated more quickly. By giving priority to applications that can be adjudicated more quickly, it improves the Department's overall average of the number of applications meeting its service standard. Additionally, there are other pressures that guide the workload to meet set targets (e.g., female and Francophone applications). The OAG's 2022 Processing Disability Benefits for Veterans audit report found that both female and French applications were taking longer on average to adjudicate than male and English applications and VAC has taken measure to address any differences.
The Department should review how they measure the length of time it takes to complete applications and how this is communicated to Veterans. In relation to meeting the service standard, the Department had fallen far below its target for a number of years. Using a single service standard does not accurately communicate to Veterans the high degree of variability there is between how applications are adjudicated. The average measure does not accurately reflect the level of work and effort that has been done to get Veterans their benefits in a more timely manner. See section 4.2.3 Service Standards for more information on this topic.
Intermediate outcome - Eligible Veterans and other individuals are recognized and compensated for the effects of service-related disabilities.
There are two components to this outcome that are measured using the National Client Survey. The survey asks Veterans if they feel the disability benefits they receive recognize their service-related disability, and whether the disability benefits they receive compensates them for their service-related disability. Results from the 2020 and 2022 National Client SurveyFootnote 16 are shown in Table 8 (PSC is broken out separately from DB).
Table 8: Intermediate Outcome Performance Measures
| 2020 | 2022 | |
|---|---|---|
| % of Veterans and other individuals who report the Pain and Suffering Compensation compensates for their service-related disability. (Target - 85%) | 63% | 57% |
| % of Veterans and other individuals who report the Pain and Suffering Compensation recognizes their service-related disability. (Target - 85%) | 75% | 67% |
| % of Veterans Affairs Canada clients who report the disability benefits they receive from VAC compensate for the effects of their service-related disability. (Target -70%) | 67% | 61% |
| % of Veterans Affairs Canada clients who report the disability benefits they receive from VAC recognize their service-related disability. (Target - 75%) | 73% | 69% |
The percentage of Veterans and other individuals who report PSC recognizes and compensates their service-related disability dropped in the latest survey and has not met the Department's target in either year. The results for the overall DB program are also less than the target and decreased in the 2022 survey. In addition, the recognition targets are not consistent for PSC (85%) and DB (75%) and should be reviewed to determine if this difference should remain (as noted in section 3.1 73% of DB clients are PSC recipients). Additional qualitative analysis of the responses between the two groups, and potential changes to performance targets would be warranted given the gap between results achieved and current targets (28% below target for some PSC measures).
Gender-based analysis plus
Table 9a below depicts first application results at the DB program level for anglophone and francophone Veterans, and Table 9b depicts results for males and females.
Table 9a: First application decision - Anglophones and Francophones
| 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|
| % of first application disability benefit decisions for anglophone Veterans completed within 16 weeks (Target - 80%) | 46% | 56% | 68% |
| % of first application disability benefit decisions for francophone Veterans completed within 16 weeks (Target - 80%) | 41% | 50% | 73% |
Table 9b: First application decisions - males and females
| 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|
| % of first application disability benefit decisions for male Veterans completed within 16 weeks (Target - 80%) | 46% | 55% | 70% |
| % of first application disability benefit decisions for female Veterans completed within 16 weeks (Target - 80%) | 44% | 54% | 65% |
In response to the 2022 Office of the Auditor General's Report on Processing Disability Benefits for Veterans the Department has placed emphasis on ensuring francophone and female applications are processed on similar timeframes as anglophone and male applications. The Department has dedicated employees to work on these applications and the results show significant improvements toward the service standard target for the above noted sub-groups. For example, for fiscal year 2023-24 the average number of weeks to process English first applications was 20 weeks, and 19 weeks for French first applications. Similarly, for fiscal year 2023-24 the average number of weeks to process female first applications was 22 weeks, and 20 weeks for male applications.
A further analysis of the 2022 client survey at the DB program level revealed that satisfaction with the level of recognition is significantly lower for Indigenous, visible minorities and serving CAF members. Chart 2 shows 59% of Indigenous Veterans feel recognized, 63% of visible minorities, and 54% of serving CAF members. There is also a correlation between age and feeling recognized, with older Veterans answering the survey questions more positively than younger Veterans.
The analysis of the question "the disability benefits I receive from VAC recognize my service-related disability" is presented in the following chart:
Chart 2: 2022 National Client Survey Results: recognition from receiving disability benefits
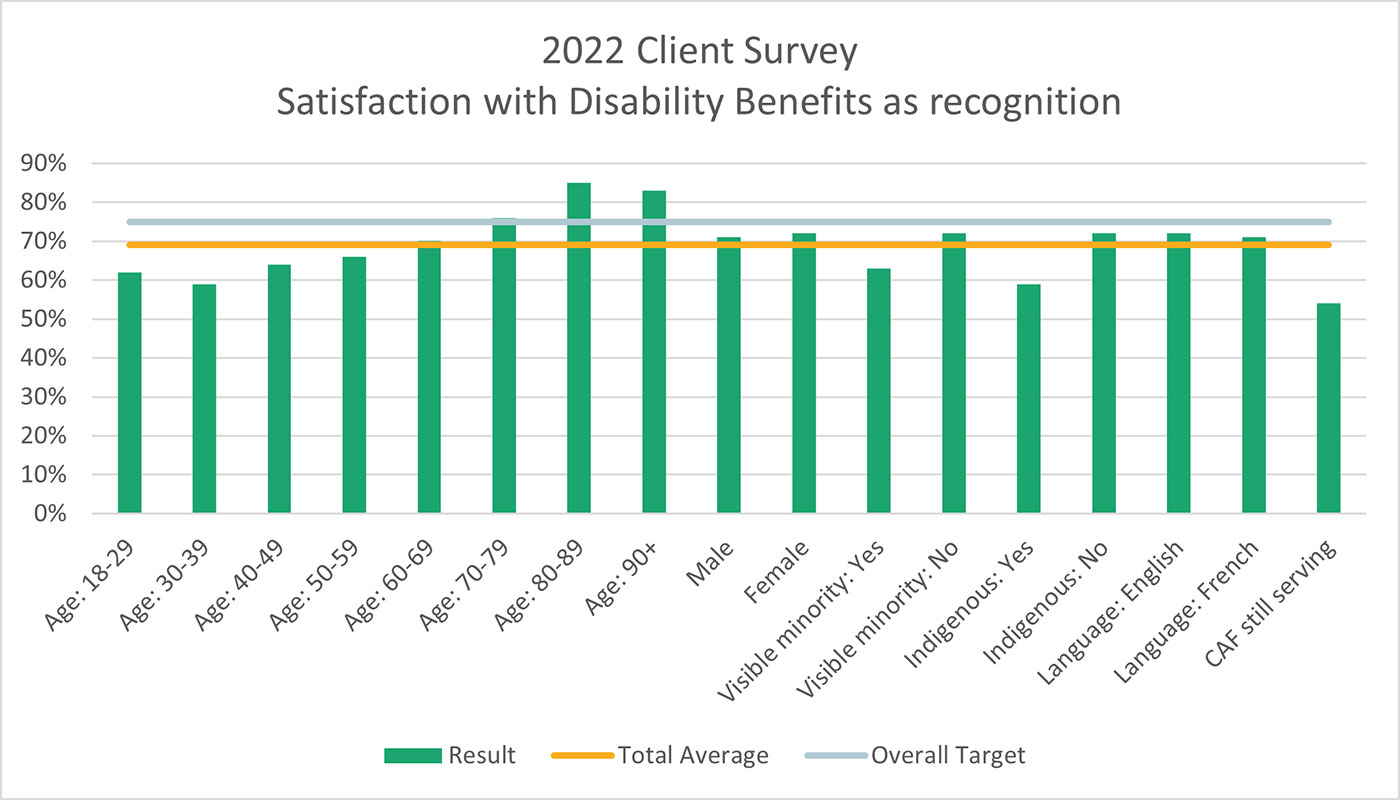
Chart 3 below shows a similar breakdown as in Chart 2 of responses of segments of clients related to the following question on the 2022 NCS: “the disability benefits I receive from VAC compensate me for the effects of my service-related disability”.
Chart 3: 2022 Client Survey Results: Satisfaction with receiving disability benefits as compensation
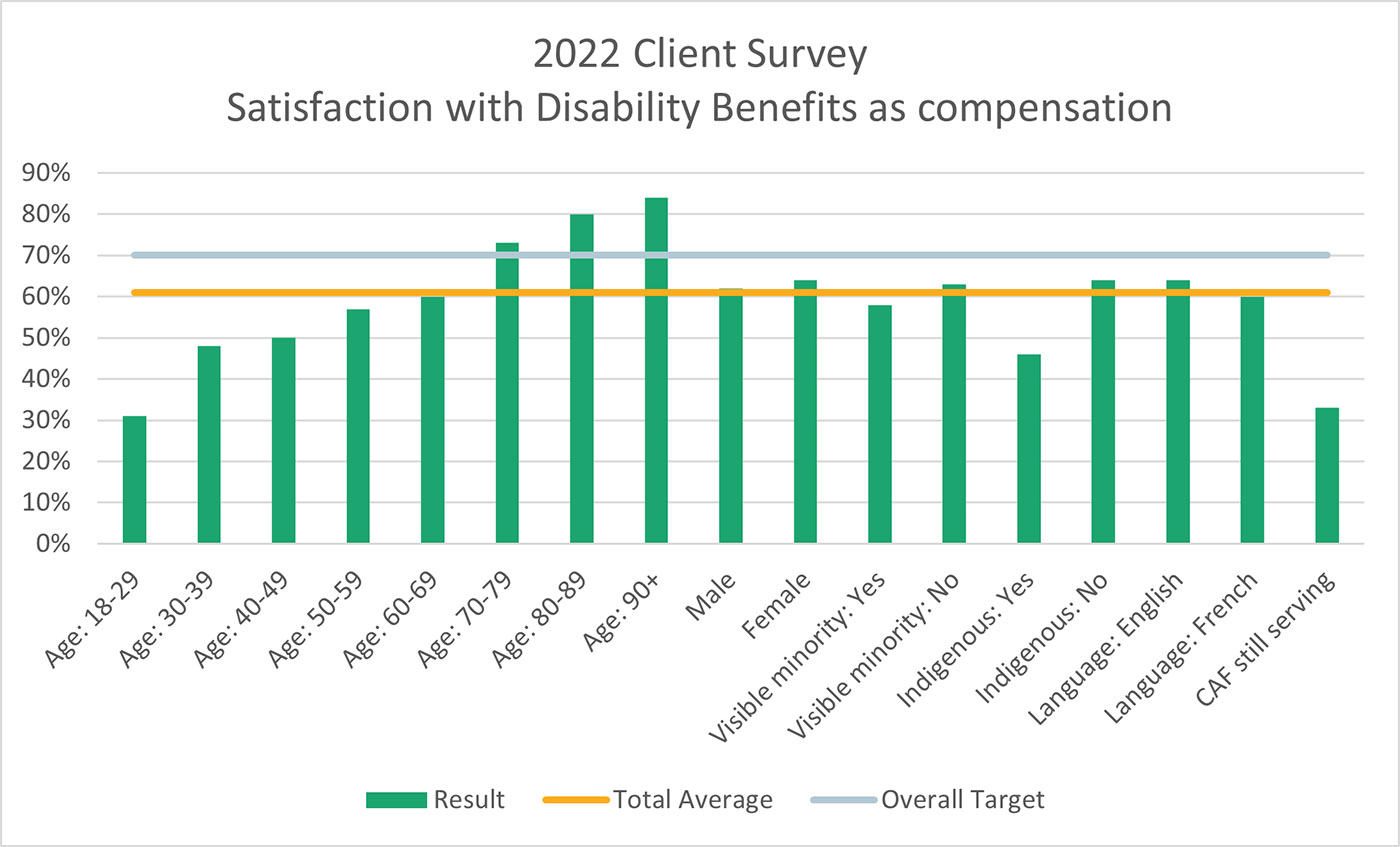
The above chart shows 46% of Indigenous Veterans feel compensated, 58% of visible minorities, and 33% of serving CAF members. There is also a correlation between age and feeling compensated, with older Veterans answering the survey question more positively than younger Veterans.
Additionally, when considering GBA plus, rates of homelessness among the Veteran population in receipt of the program can be considered. Data in VAC's CSDN showed that during the period of 1 April 2019 to 31 March 2023, there were a total of 651 DB clients who indicated to the department that they were homeless (428 of the 651 were PSC recipients). As of 31 March 2023, there were 184 DB clients whose status on the CSDN indicated they were homeless (119 of the 184 were PSC recipients).
Ultimate outcomes
There are many factors that influence progress towards, and achievement of ultimate outcomes. Neither PSC, nor DB as a whole are solely responsible for the achievement of these outcomes due to its overarching relation to Veteran health; however, the PSC and DB do contribute to these outcomes being achieved.
Ultimate outcome #1: Veterans are physically and mentally well
One of the indicators the Department uses to measure the achievement of this outcome is the percentage of Veterans who report their health as very good or excellent. The data source for this indicator recently changed from the Life After Service Survey (LASS) that was last conducted in 2019 to the Canadian Veteran Health Survey (CVHS) that was conducted in 2022. Table 10a below shows results from the final LASS and the first CVHS.
Table 10a: Ultimate outcome #1 performance measureFootnote 17 - LASS and CVHS
| 2019 | 2022 | |
|---|---|---|
| Percent of Veterans who report that their health is very good or excellent (Target - 50%) | 39% | 40% |
Sources: LASS and CVHS
The same question is also asked in the Department's National Client Survey (NCS)Footnote 18. There is a difference in the survey respondents, with the NCS surveying individuals who had recently applied for or were in receipt of VAC benefits and services. VAC has not established a target to achieve from this group of Veterans. Results from the NCS are depicted in Table 10b.
Table 10b: Ultimate outcome #1 performance measure - National Client Survey
| 2020 | 2022 | |
|---|---|---|
| Percent of clients who report their health is very good or excellent (Target - Not established%) | 27% | 21% |
Source: VAC National Client Survey
The link between the ultimate outcome, which pertains to the self-reported state of Veterans' health, and the program's intent is less obvious. The program's intent is to recognize and compensate Veterans and serving CAF members for the effects of permanent service-related disabilities, and using an indicator of health being very good or excellent does not link with the program's intent. Also, this ultimate outcome of the DB program does not align well with the immediate and intermediate outcomes, which are about recognizing and compensating for the effects of a disability.
Ultimate Outcome #2: Veterans are satisfied with the services they receive
There are two departmental results indicators to measure this outcome, and each is measured in the National Client Survey. The first indicator pertains to Veteran satisfaction with the quality of service delivery they receive from the Department. The second indicator pertains to satisfaction with the quality of programs and services offered. See Table 11 below for results.
Table 11: Ultimate outcome #2 performance measure
| 2020 | 2022 | |
|---|---|---|
| Percent of VAC clients who are satisfied with the quality of service delivery they receive from VAC. (Target - 85%) | 81% | 78% |
| Percent of VAC clients who are satisfied with the quality of VAC's programs and services offered from VAC. (Target - 85%) | 80% | 76% |
Over 75% of VAC clients surveyed were satisfied with the quality of service delivery and the quality of the programs and services VAC offers, but the target was not reached in either year, and results from the 2022 survey are trending down from the target. While the survey question does not speak specifically to DB, with DB being the largest program in terms of clients and expenditures the results would reasonably apply.
Overall, the results for PSC and DB have not been reaching the established targets. Temporary funding to support the processing of disability benefits applications has helped get decisions more quickly to Veterans, but if the funding is not renewed, VAC will see processing times increase again and less applications will meet the service standard. The number of Veterans who reported that the disability benefit they received compensated and recognized their service varied by service type, age and other factors. The evaluation found that for PSC and DB ultimate outcome #1 does not align with the program's intent to recognize and compensate Veterans for their service-related disabilities.
4.2 Program efficiency and economy
Veterans face challenges in obtaining required information in a timely manner from an overwhelmed Canadian health care system. While some measures have been taken that recognize this, a further review of application requirements and processes that considers the challenges Veterans, health care providers and departmental employees face in delivering the PSC program would be timely. The complexities should be better communicated to Veterans, and better reflected in the service standards.
4.2.1 Complexity of the program
4.2.1.1 Legislative complexity
The DB program includes recipients under PSC and DP and includes authorities from five Acts: Pension Act (1985), Royal Canadian Mounted Police Superannuation Act (1985),Royal Canadian Mounted Police Continuation Act (1970)Footnote 19, Canadian Forces Members and Veterans Re-establishment and Compensation Act (2005), Enhanced New Veterans Charter Act (2011)Footnote 20 and the Veterans Well-being Act (2018). The Well-being Act replaced the Canadian Forces Members and Veterans Re-establishment and Compensation Act and the Enhanced New Veterans Charter Act.
The acts cover multiple types of military service dating back over 100 years. The Department currently serves Veterans who served in World War II, the Korean War, during peace time service, the Afghanistan war and other Special Duty Areas, both domestic and international. The DB program also provides benefits to serving CAF members, current and former RCMP members, Veterans and family members. This means that the program needs to be able to cater to clients from different generations, each with different service experiences, and a diverse range of disabilities.
4.2.1.2 Decision-making complexity
The decision-making process for PSC is highly medicalized. VAC requires diagnostic evidence of permanent disability. This evidence is an essential component to be able to establish the link between the disability and the Veteran's service, as well as to determine the extent of the disability and impact on quality of life.
The evidence required to complete an assessment is often complex and requires specialized medical knowledge to understand. Evidence may be found in the Veteran's service health records that VAC obtains upon receipt of application, or it may become the responsibility of the applicant to undergo an assessment from a health care provider to support their application.
It is important to highlight that many employees who work within the PSC adjudication process are trained health professionals, including registered nurses, medical doctors and other health professionals. In their role they use tools that are medical in nature, such as the Entitlement Eligibility Guidelines (EEGs). The EEGs are medical and scientific evidence-based policy statements that compile current medical and scientific descriptions about certain injuries and disease, and they enhance consistency across decisions and provide for fair and unbiased decisions. VAC uses the EEGs as tools to support the first step in decision making, entitlement. VAC has an initiative underway to modernize the EEGs to support faster decisions. As of December 2023, some revised EEGs have been implemented, while work continues on others.
Another tool that supports decision makers is the Table of Disabilities (TOD). The TOD is a legislated instrument used to assess the extent of a disability for the purposes of determining disability benefits. The TOD considers the relative importance of a certain body part/system to assess the level of impairment and the impact that impairment has on the individuals quality of life. In June 2021, VAC began a multi-year initiative to modernize the TOD. The update is expected to ensure assessments reflect advances in health research and best practices. As of December 2023, several chapters have been updated and more are in progress and will be implemented as they are completed.
4.2.1.3 Healthcare system complexity
The current state of the Canadian health care system makes it more challenging for Veterans to obtain the evidence Departmental legislation and regulations requires to support their application. If the military service health records are not sufficient to support decision making a Veteran is often left to navigate the civilian health system, often without access to health care providers to provide diagnoses, complete medical questionnaires and coordinate referrals to specialists. Relocation post release, difficulties transferring medical information interprovincially, wait times to access specialists, and potentially debilitating conditions add to the difficulty Veterans experience obtaining the information needed to process their application. The Department's requirements can be a burden for both Veterans and health care providers and it adds to the time it takes for the Veteran to have a complete application that is ready for VAC to adjudicate. In response to this, VAC has been expanding the list of approved health care providers from whom VAC will accept diagnosis and medical reportsFootnote 21. Additionally, in the April 2024 federal government budget, it was announced that VAC will receive funds to expand a telemedicine initiative to provide up to two years of telemedicine services to recently released CAF members and their families.
4.2.1.4 Adjudication process complexity
Processes to adjudicate a decision can be lengthy involving several employees to work on a given application with information required from multiple sources (e.g., the Veteran or serving member, the CAF for service health records, and health care providers). Much work has been done to improve the processing times of applications, especially for the most common conditions like hearing loss, post-traumatic stress disorder and musculoskeletal conditions. In 2023-24, approximately 55% of Disability Benefits conditions completed were able to be adjudicated through a streamlined process. The remaining 45% of conditions completed were labelled as complex and required a more thorough review to be able to make a decision. Of the conditions labelled as complex, some require a medical consult by a departmental medical advisor, who assist the decision maker in determining entitlement and percentage of assessment. For more on medical consults see Section 4.2.2: Medical Advisory.
The Department has worked to overcome some of the challenges faced with the complexity within which the program operates. There are opportunities to further review requirements and processes that recognize the challenges Veterans, health care providers and departmental employees face in delivering PSC.
4.2.2 Medical Advisory
An increase in the volume of applications being sent to Medical Advisory is resulting in longer processing times for some Veterans. An increase in the volume of applications being sent to Medical Advisory is resulting in longer processing times for some Veterans.
The Medical Advisory (MA) unit within the Health Professionals Division comprises a team of medically trained employees and support staff who provide advice and support to all areas of Veterans Affairs Canada (VAC).
The specialized education, experience and knowledge of Medical and Dental advisors is used to provide expert advice and research in areas of disability medicine. Medical and Dental Advisors support the Disability Adjudication team with disability entitlement and first assessment decisions along with disability reassessment decisions. The Paramedical Team in the Medical Advisory Unit provides direct assistance and support to clients in navigating the disability reassessment process.
Representatives from the MA unit also participate on departmental committees and provide guidance and advice in the development, revision, and medical interpretation of VAC policies and processes.
4.2.2.1 Role of Medical and Dental Advisors
One of the roles of the Medical and Dental advisorsFootnote 22 is to support the DB adjudication process. Depending on the experience of the adjudicator, and when applications include health conditions with a higher level of complexity, the adjudicator may ask for a diagnostic clarification, a medical opinion or they may require the medical professional to provide the disability assessment for the health condition the Veteran applied for.
4.2.2.2 Workload Management and Consultation Time within Medical Advisory
The MA unit manually tracks the number of consults they receive and complete, to assist with workload management. This was due to reporting functionalities of the new GCcase system (used to process most PSC applications) being incomplete, and there were challenges with system generated reports not capturing the complete workload (from both CSDN and GCcase).
Throughout the course of the evaluation, system generated reporting capabilities improved. At the time of report writing, system generated data outlining the number of MA consults received, completed, and pending from 1 April 2022- 31 July 2024 became available. As the evaluation team compared and contrasted the manually tracked data (relating to MA consults) to the system generated data (relating to MA consults) the team noted discrepancies in the counts of the number of consults. In interviews with the medical advisory and the centralized operations reporting units, it was determined that the differences could exist for a number of different reasons such as: incomplete GCcase consult data in the early years of PSC; the differences in reporting that occur when reporting the number of health conditions requiring consults versus the number of applications requiring consults; and finally manual spreadsheet tracking of information versus system generated tracking.
In order for the evaluation team to better reflect the historical increases in medical consults requested, the evaluation team analyzed both the manually tracked the number of consults (31 March 2021 to 31 March 2022) as well as the newly developed system generated reports tracked by fiscal year from 1 April 2022 to 31 July 2024.
As can been seen in Chart 4 below, there has been a significant increase in the volume of work coming into MA (Consult Requests), and this has led to a steady increase in the number applications awaiting a medical consult (Consults Pending). Chart 4 shows the number of consults pending within MA have significantly increased, from 151 in March 2021, to 2,462 in July 2024.
Chart 4: MA workload
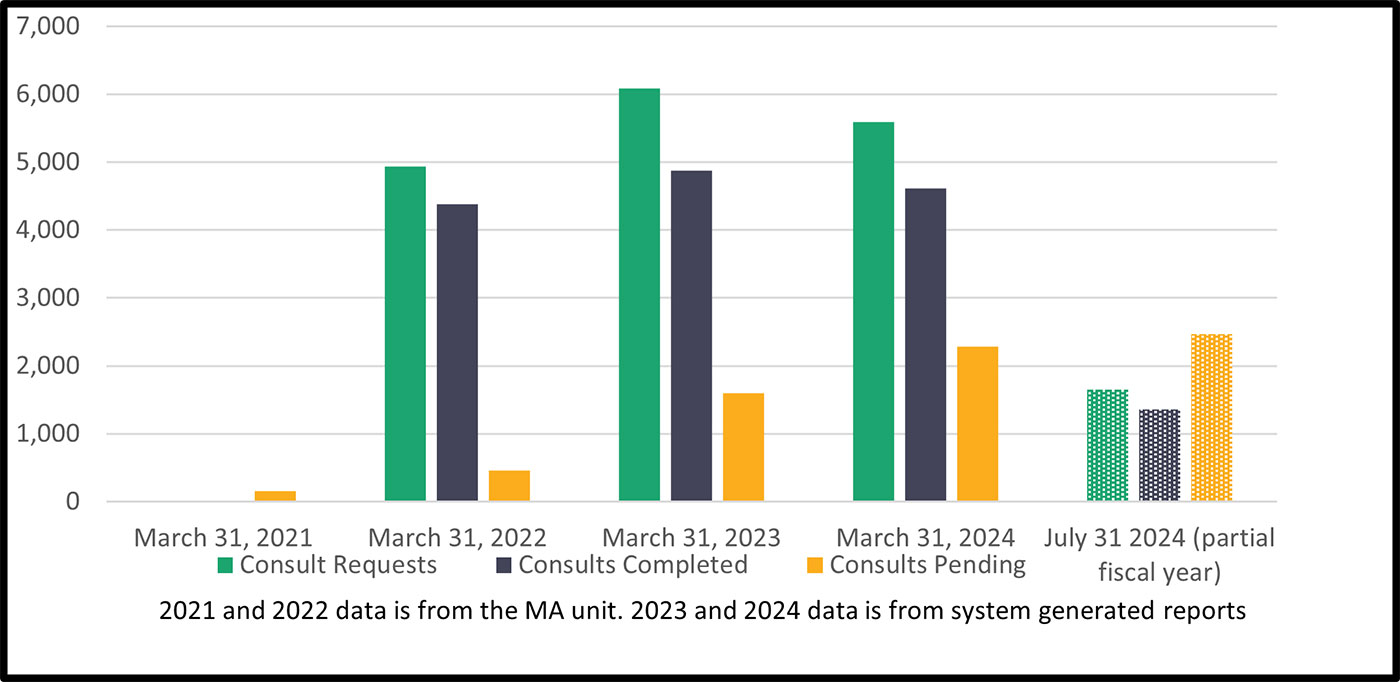
Factors contributing to the increase in applications awaiting medical advisory consult can be attributed to: many new adjudicators hired during the evaluation scope period led to more applications processed and therefore more requests for medical consults (with some medical consults being the result of lack of training and experience of the new adjudicators); the complexity of cases; and challenges ensuring the unit is staffed to meet the volume of workFootnote 23. As the number of applications in MA awaiting a consult continues to grow, the Department needs to consider ways to manage this component of the adjudication process to ensure Veterans are receiving timely decisions (i.e., applications are completed within the 16 week service standard). The evaluation team analyzed system data during the scope period and this information showed the average number of weeks from when the consult was requested to when the consult was completed ranged from 12 weeks over the 2020 calendar year to 22 weeks in 2024 (as of 3 June 2024).
Interviewees indicated that the MA team is also receiving requests for consultation that should be dealt with at the adjudicator level. This was supported by two reviews conducted by VAC's Centralized Operations Division, in September and October 2023, in which Disability Consultants reviewed a sample of applications that were sent to MA. Disability Consultants are experienced adjudicators that provide training, coaching and assistance to decision-makers. As a result of the reviews, approximately one-third of the medical consult requests in the samples were pulled back and returned to the decision-maker to make the decision based on the evidence in the file. This was an opportunity to provide additional training and guidance to adjudicators. Interviewees stated reasons for claims being sent to MA include adjudicators wanting to have another person review the claim before making a decision, not using the training and tools available to the adjudicator, pressure to meet performance targets, many new adjudicators, and a lack of training on the medical condition.
The Department has been busy training new decision-makers and expanding the knowledge of more experienced decision-makers. With more decision-makers trained to assess more types of health conditions, along with more experience adjudicating applications; the expectation is that less applications will need to be sent to MA. Decision-makers are expected to first consult with Disability Consultants when they need advice or assistance, and doing so will keep some applications from going to MA. Given the outcome of the reviews, it would be beneficial to conduct periodic reviews of medical consult requests sent to MA, which will alleviate unnecessary applications sitting in the MA queue.
As the Department works to enhance the training of Disability Adjudicators as outlined in the paragraph above, the MA unit needs to develop a plan to reduce the number of applications awaiting consult. To expedite consults, the MA unit has been focusing on specific types of applications, as well as having the medical advisors focus on consults exclusively one week per month (i.e., taking them off other work they perform). While these initiatives are beneficial, more may be required in the short term to reduce the volume of applications awaiting a consult. Also, the absence of complete and accurate data relating to medical consults needs to be addressed.
4.2.3 Service Standards
VAC has committed to adjudicate 80% of disability benefit first applications and reassessments within 16 weeks of receiving a complete application. However, this service standard does not take into consideration whether the application is complex or straightforward, or the number of conditions within one application. The Department should better communicate to Veterans how long they can reasonably expect to wait for their decision and consider modifications to current service standards.VAC has committed to adjudicate 80% of disability benefit first applications and reassessments within 16 weeks of receiving a complete application. However, this service standard does not take into consideration whether the application is complex or straightforward, or the number of conditions within one application. The Department should better communicate to Veterans how long they can reasonably expect to wait for their decision and consider modifications to current service standards.
Service standards are integral to good client service and to effectively manage performance. They help clarify expectations for clients and employees, drive service improvement, and contribute to results-based management. Service standards reinforce government accountability by making performance transparent and increase the confidence of Canadians in government by demonstrating the government's commitment to service excellence.
Service standards serve two key purposes:
- To provide employees with performance targets (e.g., phone calls must be answered within two minutes);
- To inform clients what to expect (e.g., the current wait time to have your call answered is less than five minutes).
VAC has service standards for most programs, including the DB program. VAC also has a service pledge that is outlined on its external website regarding the Department's values and ethics principles. It states “we take pride in our role as public servants and are dedicated to service excellence. We are committed to responsive, quality service, delivered with timeliness, courtesy and fairness”.
A 2017 consultant's reportFootnote 24 that reviewed VAC's service standards noted that:
"an organization's service standards establish a very public commitment for delivering its most important services in both a timely and high-quality manner while ensuring clients have ready access to these key services. They ultimately define how clients can expect to be treated by the organization. As such, service standards need to be established with care and thoughtfulness and must also consider both the current and expected services volumes and supporting resource requirements necessary to maintain the stated service levels described by these published standards."
As indicated in Section 1.5, the published service standard for processing PSC and Disability Pension first applications is 16 weeks 80% of the time. The purpose of the 80% target is to help manage operations and track progress against overall delivery objectives. In general, targets take into account the risks associated with process delays and uncertainties arising from factors such as workload fluctuations, employee turnover, and seasonal variations.
In the past, VAC has changed the service standard. Changes include the date that the Department started measuring the standard, the overall length of time of the standard, and the service standard end date. The start date has evolved from date of application request to the date VAC has received a complete application. For example, in 2008-09 the service standard was 24 weeks from the date of application to the decision date. In 2011, VAC adjusted the service standard to be 16 weeks from the time VAC received a complete application to decision date. For fiscal year 2014-15, VAC adjusted the standard from 16 weeks to 12 weeks and achieved this for 64% of DB applications. This was done prior to the increase in applications that started in 2015-16 (see Table 5). As the Department was unable to achieve the 12-week service standard with this rise in applications it reinstated the 16-week service standard in 2015-16. In the 2022 Auditor General of Canada's (OAG) Processing Disability Benefits for Veterans report there was a recommendation to amend the end date for the service standard to include the time from decision to payment verified date (for favourable decisions). This change was made in April 2022. For more details on the OAG recommendation, see Appendix AFootnote 25.
VAC has been under scrutiny for several years as the Department has been unable to regularly meet its 16-week service standard. The number of DB applications outside the 16-week service standard grew to over 22,000 by the end of the 2019-20 fiscal year. This is due, in large part, to a significant increase in applications for disability benefits. As indicated earlier in this report, the Department has put measures in place to decrease the backlog including implementing changes to processes, hiring more adjudicators and developing new ways to streamline the adjudication process. The result has been VAC moving closer to meeting the 80% target for completing first applications within 16 weeks. For fiscal year 2023-24, 76% of PSC first applications were completed within 16 weeks (69% for all DB first applications). Based on an 80% target, VAC is communicating an expectation that there will be 20% of applications taking longer than the 16-week service standard.
Although progress has been made towards achieving the target for the 16-week service standard, there are challenges with the service standard itself. The standard is a single measure where there are multiple types of applications, multiple client types, multiple adjudication processes, and varying levels of complexity for a wide range of medical conditions that Veterans are applying for. There have been and continue to be internal and external pressures to continue to improve performance against the service standard. Veterans' organizations, politicians, and the media have highlighted that Veterans have been frustrated with the length of time it has taken to get their decisions, and the lack of clarity on how long it will take to process their applications. Interviews with VAC employees noted challenges in explaining the process and delays to Veterans and managing Veterans' expectations.
Applications are supposed to be adjudicated in chronological order, with the oldest complete applications being processed firstFootnote 26. However, there are instances where the processing of applications has been directed in ways to process more applications to meet production targets (including the service standard). This has resulted in more Veterans getting a decision in less than 16 weeks, while there remains a number of older applications yet to be adjudicated. For example, reassessment applications can be processed quicker than first applications, so the Department has directed employees at times to work on reassessments for a period of time. Also, VAC has put emphasis on training employees in the conditions that have the highest volume of applications (hearing loss, musculoskeletal conditions and post-traumatic stress disorder), resulting in Veterans receiving a decision faster for these conditions than Veterans applying for other medical conditions. These practices can lead to inaccurate expectations for Veterans who are applying for conditions that are not among the most common, and for conditions that are deemed complex as these types of claims may fall outside of the overall average processing times. Applications deemed complex often take longer, but VAC does not adequately communicate this to Veterans. Treating all first applications and reassessments as equal in terms of the service standard can lead to frustration for some Veterans. The average of all first applications is what VAC measures and reports on, and this neither accurately reflects the time a Veteran can expect to wait, nor does it reflect the one-third of applications that were adjudicated in less than eight weeks, between April 2022 and January 2024.
4.2.3.1 Workload reporting
Interviewees noted that the Department is currently considering an opportunity to report results by medical condition applied for, rather than the current practice of reporting at the application level. Prior to the implementation of GCcase, the Department only had the ability to report on the program at the application level. The Department has been considering making this change to better reflect the workload and the results.
VAC reports internally on the DB program in two ways: 1 - at the application level and 2 - at the condition level.
- At the application level, VAC can only report one favourable rate and one processing time, even though there may be multiple conditions on one application that can be processed separately.
- At the condition level, each condition the Veteran applies for is treated individually in terms of having its own processing time and favourable or unfavourable decision.
When a Veteran applies for multiple conditions on a single application, the conditions are often adjudicated separately, and the Veteran will receive a decision letter and payment (if favourable) for the individual conditions on the application. However, when reporting against the service standard at the application level, the service standard is not considered met until all of the conditions have been adjudicated.
The discrepancy in reporting is especially noticeable when a Veteran applies for both a condition that is straightforward to adjudicate (e.g., hearing loss) and a complex condition that requires more effort to adjudicate (e.g., neurological or digestive system conditions). The turnaround time for both conditions against the 16-week service standard is dictated by the condition that takes the longest to complete. So, if the straightforward condition takes 10 weeks to adjudicate and the complex condition takes 30 weeks to adjudicate, the application, and each condition within the application is considered to have taken 30 weeks to complete even though the Veteran received a decision and payment after 10 weeks for the straightforward condition.
The other area this change will impact is the favourable rate for decisions. From April 2023 to January 2024 the favourable rate at the application level for DB first applications was 77%. Internal reports at the condition level (which means considering each condition applied for individually) show that for fiscal year 2023-24 the favourable rate was 67%. This difference in reporting of favourable rates does not change the outcomes for Veterans, just how the results are reported. For example, if a Veteran applies for three conditions on a single application, and the Veteran receives a favourable decision for one of the conditions, the whole application is deemed to have been favourable. With a move to reporting at the medical condition level, there would be one condition reported as favourable, and two conditions reported as unfavourable.
The number of decisions remains the same, and the results remain the same for the Veteran, but the reporting of the results could be more representative of the workload and the decisions communicated to Veterans.
There are challenges when reporting at the application level as there can only be one service standard start date for the application, but there may be instances where various conditions have already been adjudicated on before the whole application is considered a complete application. The evaluation team did not make a recommendation between the two methods of reporting (via condition or via application) and suggest the program and reporting groups continue to discuss options to ensure the most relevant and accurate information is available to be reported on. Currently, reporting internally and externally in multiple ways (e.g., some by condition and some by application) can be confusing in understanding the performance of the program.
4.2.3.2 Service standards in other government departments
Other government departments have multiple service standards for benefits or services. The evaluation team reviewed service standards from three government departments and agencies and found that more details and more specificity are provided to applicants and Canadians on what they can expect, and what the recent performance has been for the benefit or service. VAC is lacking specificity in its service standards related to the DB program. By providing more details to Veterans about the length of time they can expect for their application type, it would provide a more accurate representation of how long Veterans can expect to wait to get a decision. See Appendix B for more details of service standards for other government departments.
4.2.4 Incomplete applications - Withdrawn or on-hold applications
Veterans can submit applications to VAC multiple ways: 1 - electronically via My VAC Account (MVA), 2 - by completing a paper copy of the application form and mailing it or dropping it off to a VAC or Service Canada office or 3 - through a representative of the Royal Canadian Legion. Over the last several years, VAC has encouraged Veterans to apply via MVA, and the Department has made enhancements to MVA to facilitate this, including having a guided web formFootnote 27 to assist with the application process.
While MVA does make the application process easier by allowing Veterans to submit their application electronically, MVA allows applications to be submitted that are missing required informationFootnote 28. In MVA, the form does not clearly indicate all of the information that is required to process an application. For example, Veterans are asked if they have a medical diagnosis for their condition. The Veteran is asked to answer Yes or No. The Veteran can answer No and keep proceeding with the application and submit it to VAC. The Veterans' MVA will show the application as being in-progress. However, a medical diagnosis is a requirement for VAC to make a decision and additional medical information is needed before the application can proceed to be adjudicated. This will add time to the processing of the application for which Veterans may not be aware at the time of application submission. VAC employees work with the Veteran and health care providers to obtain information to allow the application to be adjudicated.
The relative ease of submission could be one of the reasons the Department is receiving a significant number of applications that are missing information required for processing (as of 30 September 2023 VAC reported there were 15,730 pending incomplete applications). VAC reports that many of these are due to missing signatures, proof of identity or required medical questionnaires, but it also includes a lack of diagnosis.
For applications that are submitted via MVA the Veteran can log into their account and see their application status as “in-progress”. These “in-progress” applications are assigned to a VAC employee who will review the application for completeness and order the Veterans service health records from the CAF or from Library and Archives Canada. Due to the high volume of applications being submitted, it may take several weeks before the application has the initial review by a VAC employee. If information is missing, the application will not continue to be processed at that time. VAC will notify the Veteran of any missing pieces of information, via a letter that is mailed to the Veteran or uploaded on MVA. The letter to the Veteran indicates that they have 60 days to send in the required documentation or the application will be placed on hold. In some instances 60 days may not be enough time for some Veterans to get the information required, and notifying Veterans that their application has been put on-hold/withdrawn before they can send in the information has the potential to be frustrating for Veterans. It is a good practice to inform the Veteran that information is missing from the application; however, the 60 day timeframe has fluctuated over the years, and in reality the number of days VAC gives the Veteran to send in the information is arbitrary and is mainly a method for managing the workload.
If the documentation is not received by VAC within 60 days the Veteran will be notified that their application is being placed on-hold. The application is removed from the Department's workload queue and from the number of applications being reported as pending or in-progress. Rather than have a 60-day timeframe, the application should be immediately placed on-hold and the Veteran notified of the information that is missing. Whenever the information is received, VAC will reinstate the applicationFootnote 29.
VAC does not count the time period that the application is deemed incomplete within the 16-week service standard. For favourable decisions, it is important to note that the date of application is used to determine when payment of the disability benefit begins, even if the application was placed on hold and removed from the in-progress/pending queue at some point in the adjudication process. A complete application is considered by the Department as the service standard start date.
4.2.4.1 Reporting on incomplete applications
VAC records, tracks and reports on the number of applications received. Each application submitted is recorded as “received”, whether that application is complete with all required information or incomplete. Incomplete applications are part of the Department's workload as the Veteran has submitted an application and is expecting a decision. The number of DB applications received is compared against the number of applications completed (depicted as Difference in Table 12 below). For at least the past six fiscal years, the number of received applications has always been higher than the number of completed applications (see Table 12 below). This gives the perception that VAC is not processing as many applications as it receives; however, while this is true, it is not a fair comparison due to the volume of incomplete applications that VAC records as received that cannot be completed without additional information. The way VAC is reporting applications received is overstating the volume of applications that are able to be adjudicated.
As depicted in Table 12 below, VAC has significantly increased the number of applications completed and placed on hold/withdrawn since 2020-21.
Table 12: Overview of DB applications
| 2018-2019 | 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|---|
| Applications received | 60,975 | 62,892 | 45,500 | 66,255 | 72,575 | 80,256 |
| Applications completed | 41,783 | 42,255 | 40,615 | 56,103 | 51,182 | 55,729 |
| Difference | 19,192 | 20,637 | 4,885 | 10,152 | 21,393 | 24,527 |
| Applications withdrawn | 10,428 | 15,340 | 12,004 | 24,370 | 23,064 | 25,508 |
| Increase (decrease) in pending applications | 8,764 | 5,297 | (7,119) | (14,218) | 1,671 | (981) |
| Total of completed plus withdrawn | 52,211 | 57,595 | 52,619 | 80,473 | 74,246 | 81,237 |
To reconcile the difference in applications received and applications completed, VAC counts applications put on hold (e.g., incomplete applications) as withdrawn in its workload reporting. The number of applications withdrawn has increased significantly, both in terms of numbers and percentage of applications received (17% of applications received were withdrawn in 2018-19 while 31% were withdrawn in 2023-24)Footnote 30.
There is an opportunity for VAC to reconsider how applications are recorded, tracked, reported and communicated on to more accurately reflect the workload, and the number of applications in-progress/pending, to better communicate with Veterans the status of their applications. A more accurate measurement for reporting and comparison would be to compare the number of applications that have all the information needed to be adjudicated against the total number of applications that received a decision (i.e., completed).
4.2.5 Technology, Systems, & Digitization
Much work has been done to modernize VAC's IT systems; however, much work remains to have a single user interface that is able to process all disability benefit applications from intake to payment and provide consistent data for program decision making.
The evaluation team reviewed documentation related to the IT systems that support PSC, from the initial implementation phase of PSC in 2019 to the IT modernization phase which continues today.
To support the delivery of the new PFL programs, modernization of systems/digitization was undertaken. These changes supported the overall implementation of the program, improved service to Veterans and their families, and provided some efficiencies and support for frontline employees.
4.2.5.1 System Replacement and Digital Transformation
In 2019 VAC made improvements to MVA that included a streamlined single online application process, and guided forms to make filling out VAC applications easier while collecting more accurate data directly from the user. Another improvement was the addition of application status tracking functions in MVA that provide notifications to Veterans as applications move through the various steps of the adjudication process.
Applications submitted through MVA are uploaded directly to GCcase for processing. However, due to system limitations, many applications must be manually transferred to CSDN to be adjudicated. Between 1 April 2019 and 13 December 2023, 33,620 health conditions were transferred (withdrawn and reinstated) from GCcase to CSDN.
The manual transfer of these files from GCcase to CSDN triggers two status change notifications to Veterans via MVA. The first change notification informs Veterans that their application was withdrawn, with the following message: “Do not worry, the processing of your application has not been affected. The withdrawn status is only showing because of a change in our administrative process. Your application will be re-instated automatically and will appear as a duplicate in this list”. The second notification shows the application was reinstated; however, the withdrawn notification remains visible on MVA. The actual manual transfer of the files takes employees anywhere from just a few minutes to potentially up to 45 minutes depending on the volume of information that has to be transferred. However, due to the volume of applications that need to be transferred from GCcase to CSDN, the applications will wait 2-3 days (and sometimes up to one week) before the employees perform the transfer from GCcase to CSDN (this time is counted against the service standard).
There is no need for Veterans to receive the notifications that are highlighting an internal administrative process. Interviewees stated that the application status tracking functionality in GCcase cannot suppress these notifications unless all notifications are turned off. Some interviewees indicated that the MVA messages are confusing, and lead to inquiries from Veterans as to why their application was “withdrawn”. This is an issue that needs to be addressed in the short term.
In addition to MVA changes, VAC also planned to replace its legacy CSDN application processing system with GCcase, a system that was aligned with the Government of Canada's digital strategy. GCcase launched in 2019, however, it has not yet been fully developed and as a result CSDN is still needed to both adjudicate certain application types that are more complicated to process, and for payment processing of all applications.
While there are benefits to using GCcase, many employees are required to work in two systems with different functionality, look and feel, and capabilities. The lack of a single system continues to lead to prolonged training for staff, more workarounds to be able to process applications, and longer processing times for certain medical conditions. From a reporting standpoint, there are challenges with applications being transferred between GCcase and CSDN, having data being input into two systems and the ability to generate accurate reports.
Changes to processes had to be made to keep applications moving through the two adjudication systems. In addition, training new employees on dual systems has been time consuming and challenging for the Department. The situation adds complexity to the adjudication process that consumes additional resources from both operations and from IT. This impacts Veterans who are waiting for their application to be adjudicated (i.e., increases processing time).
The replacement of CSDN is ongoing as outlined in VAC's current IT Modernization Plan. The objective of one single easy to use client centric application processing system has not been realized five years since GCcase was implemented.
4.2.5.2 Current Status
VAC has made progress in implementing the system updates proposed under PFL, helping to modernize and streamline the benefit application process for Veterans; however, the complexities of transitioning from a legacy system have proved challenging. Employees continue to work in and express frustration in having to work in two unique systems on a daily basis.
Starting in 2023-24, VAC began a sizable, two phase, department-wide IT Modernization project that would be implemented over five years. This includes objectives such as replacing CSDN and implementing modern payment processes over the five-year timeline.
There are, however, situations where immediate improvements are required that could benefit Veterans and employees, as opposed to five years from now, such as eliminating the withdrawn notification Veterans receive when VAC is just transferring applications from GCcase to CSDN. A change such as this could save Veterans undue stress, reduce workload and reduce unnecessary contact with the Department. If there are changes that can prevent or reduce stress and/or negative experiences with VAC, the IT changes should be made a priority.
Issues that have or will impact a Veteran's experience in a negative way and can be avoided/corrected with limited intervention should be actioned quickly regardless of any large-scale multi-year projects. Improving service can take the form of being more precise in communications, making language improvements in our automated correspondence and other types of short-term corrections that can either reduce stress, improve the experience, or avoid confusion and frustration for Veterans. These can have an immediate impact on numerous Veterans between now and when the IT Modernization project is expected to be completed. For example, work has been done to improve the application form and how the department communicates what is required for a DB application to be deemed complete. There is a systems component to this and program management and IT should collaborate to ensure these changes get implemented. Additionally there are system enhancements waiting to be worked on that have not gotten priority to be actioned.
While these improvements will support a better experience for Veterans and front-line employees, VAC's IT Modernization project remains the top priority. It identifies the requirement for modernization due to outdated technology, lack of developer support for legacy systems (e.g., CSDN), burdensome user experience, gaps in reporting functionality, and the inability to update to current accessibility standards. Modernization of this aging IT aligns with the Government of Canada Digital Standards and the Policy on Service and Digital. Remaining nimble enough to ensure maintenance and improvements to our current systems are not delayed for excessive amounts of time, will improve VAC's ability to better serve Veterans.
4.3. PSC Expenditures
Program expenditures for PSC have increased by 76% from 2019-20 ($917 million), to 2023-24 ($1.61 billion). During this same timeframe, overall spending on DB grew by 10%, from $2.47 billion in 2019-20 to $2.74 billion in 2022-23, with expenditures in 2023-24 forecasted to decrease by 2% to $2.42 billion. For 2023-24, PSC is forecasted to account for 67% of overall DB expenditures, up from 37% in 2019-20.
Over the past several years, VAC has received temporary funding for additional resources in order to address the volume of applications awaiting processing and to modernize services. In April of 2018, VAC had approximately 185 employees primarily focused on disability benefit operationsFootnote 31 (i.e., decision makers, payment officers, intake officers and disability consultants; does not include management or employees working in DB program management). Over the next four years, temporary funding allowed for additional hiring, with the number of employees (decision makers and support staff) reaching a high of over 650 in 2020-21. As of March 2024, VAC had 460 employees dedicated to DB operations. The number of employees fluctuated over these years as the funding was temporary and employees left for other opportunities. The addition of the temporary employees over the past five years has enabled VAC to reduce turn-around times on first applications from 49 weeks in 2020-21, to 19 weeks as of 1 December 2023. As a result, the DB backlog was reduced from more than 22,000 applications in March 2020, to approximately 5,600 as of March 2024.
The following chart demonstrates that over the past five years VAC has been able to significantly increase the number of applications it processes with the help of additional resources, resulting in a reduction to the backlog and improved turnaround times.
Chart 5: Resourcing and associated impacts on application processing

As recommended in the 2022 OAG's Audit of Processing Disability Benefits for Veterans, the Department developed a plan to secure more permanent resources to reduce the processing times for individuals applying for DB. VAC put forward a 2023 budget proposal in response to the audit recommendation for permanent resources; however, this was not funded in the federal budget. Instead, in November 2023, the Minister of Veterans Affairs announced an extension of the temporary resources for an additional two years, from 1 April 2024 to 31 March 2026.
While VAC has been able to leverage temporary funding to address the backlog and improve efficiency, the Department has yet to secure additional permanent or long-term funding to continue to meet the demand for DB. The forecasted demand for DB (as depicted in Chart 1) supports the need to continue with additional employees, and process and system modernization, to ensure service standards are being met. With streamlined processes and system modernization, along with a robust forecast of demand the department will be better able to identify and validate what long-term resources are needed to support the demand for DB into the future.
5.0 Conclusion
The DB program has been VAC's signature program for many decades, and is often the program for which Veterans first apply for benefits from the department. PSC is the most recent evolution of the compensation offered that provides recognition to Veterans and serving CAF members for permanent service-related disabilities. The evaluation team found that there is a continued need and an ongoing high-level of demand for compensation through PSC. Over the past several years, the number of annual applications received has continued to increase, and VAC has responded by completing more applications, resulting in more Veterans receiving their compensation and recognition. The number of applications that are outside the 16-week service standard has significantly decreased from its peak in 2020.
The PSC aligns with government priorities and federal government roles and responsibilities.
A number of initiatives have been implemented or were in-progress over the scope of the evaluation to enhance the effectiveness and efficiency of the DB program. There is performance information available to support the evaluation; however, most targets are not being reached, with segments of the Veteran population reporting much lower rates of feeling compensated and recognized through their PSC benefit. The ultimate outcome is not an appropriate measure of the PSC benefit, and there is significant overlap in the intermediate outcomes.
There are various types of applications (first applications, reassessments and departmental reviews) that VAC receives, with some being straightforward to process and some very complex. Based on the type of application, new service standards are needed to better communicate with Veterans how long they can reasonably expect to wait for a decision.
There remains significant challenges related to the IT systems employees use to process applications. The goal of replacing CSDN with a new system has yet to be realized, five years since GCcase was implemented. This has impacts on Veterans and employees who must work in two separate systems, with workarounds needed in order to process applications, and this takes extra resources and adds time to process applications.
The addition of multiple rounds of temporary funding has helped get Veterans their decisions in a more timely manner than when the backlog was at its peak. The department is processing thousands more applications per year than it was five years ago, and payments to Veterans are higher than at any point in the department's history. In order to maintain this momentum, VAC should continue to find greater efficiencies through more streamlined processes and IT modernization. With these adjustments, and a formalized forecast of demand, the department could then more effectively assess the amount of long-term funding needed to ensure applications are processed efficiently, with modernized processes, and in a timely manner.
6.0 Recommendations
Recommendation 1:
It is recommended that the Assistant Deputy Minister, Service Delivery, in collaboration with the Assistant Deputy Minister, Chief Financial Officer and Corporate Services develop a Disability Benefits strategy that will enhance the efficiency and experience of the program for both Veterans and employees and build program sustainability. A corresponding action plan will include actions that:
- Streamline workflows and business processes.
- Review and update process requirements, as appropriate, with consideration of the administrative burden on clients, employees, and the Canadian Health Care system.
- Enhance processing through an innovative technology solution that can address disability benefit applications from intake to payment through a single window interface for users.
Management Response: Veterans Affairs Canada agrees with the recommendation.
| Action and Rationale | Expected Completion /Implementation Date | ADM Accountable for Action |
|---|---|---|
| To best position the Department to meet ongoing demand for Disability Benefits within service standards*, a two-phased approach will be initiated: * As of July 2024, the date when the evaluation was substantially completed, Veterans Affairs Canada's service standard for disability benefit applications was 16 weeks for first applications 80% of the time. Phase 1: A cross-functional team will complete a critical analysis of the current state of Disability Benefits administration and develop recommendations for an effective, efficient, and stable future state that is in alignment with Veterans Affairs Canada's strategic plan and the projected growth in demand for Disability Benefits. This analysis will result in a strategy in alignment with departmental service modernization efforts led by the Chief Digital Service Modernization Office. Phase 2: In consultation with the Chief Digital Service Transformation Office, an action plan will be developed to address the issues identified in the strategy to include deliverables, timelines, and resource requirements. The plan will reflect the intent of Service Modernization Strategy and the Service Modernization Workplan. Implementation efforts will be contingent on the outcomes of Budget 2025 and the Refocusing Government Spending exercise. |
March 31, 2026 | Assistant Deputy Minister, Service Delivery |
Recommendation 2:
In conjunction with Recommendation 1, to ensure smaller scale pressures on the disability benefits program are addressed it is recommended that:
- The Director General Centralized Operations Division, in collaboration with the Director General, Service Delivery and Program Management and the Director General, Information Technology, Information Management, Access to Information and Privacy (ITIMAP), ensure system related process improvements are identified, communicated, and prioritized to support efficient delivery of disability benefits.
- The Director General, Centralized Operations Division continue to invest in adjudicator training and monitoring of medical advisory requests with a view to ensuring only necessary conditions are sent for a medical consult.
- The Director General, Health Professionals Division ensure that the appropriate processes and resources are available to both reduce the current number of applications awaiting a consult, and provide a timely response to future medical consult requests.
Management Response: Veterans Affairs Canada agrees with the recommendation; however, Health Professionals Division notes that recruitment of Physicians can be challenging.
| Action and Rationale | Expected Completion /Implementation Date | ADM Accountable for Action |
|---|---|---|
|
#2(a)
#2(b)
#2(c)
|
October 31, 2026 September 30, 2026 September 30, 2026 |
Assistant Deputy Minister, Service Delivery Assistant Deputy Minister (ADM) Chief Financial Officer and Corporate Services Branch Assistant Deputy Minister, Service Delivery |
Recommendation 3:
It is recommended that the Director General, Centralized Operations Division, in consultation with the Director General, Strategic Planning, Results and Cabinet Business, develop transparent Veteran-focused service standards with consideration of the different types of applications and adjudicative processes.
Management Response: Veterans Affairs Canada agrees with the recommendation.
| Action and Rationale | Expected Completion /Implementation Date | ADM Accountable for Action |
|---|---|---|
|
Upon finalizing the DB strategy with the goal of positioning the Department to meet ongoing demand for DB within service standards (Recommendation #1), the Director General, Centralized Operations Division, will work in consultation with the Director General, Strategic Planning, Results and Cabinet Business to:
|
December 31, 2026 | Assistant Deputy Minister, Service Delivery in collaboration with ADM, Strategic Policy, Planning and Performance |
Recommendation 4:
- It is recommended that the Director General, Centralized Operations Division, in consultation with the Director General Strategic Planning, Results and Cabinet Business review outcomes, results and targets with a view to ensuring they are aligned with the objective of the program and are achievable.
- It is recommended that the Director General, Policy and Research determine why outcome achievement is significantly less for segments of the client population.
Management Response: Veterans Affairs Canada agrees with the recommendation.
| Action and Rationale | Expected Completion /Implementation Date | ADM Accountable for Action |
|---|---|---|
|
#4(a) The Director General, Centralized Operations Division, will work in consultation with the Director General, Strategic Planning, Results and Cabinet Business to:
#4(b) With respect to Recommendation 2(b), the evaluation identified two questions from the 2022 VAC National Client Survey where specific segments of the population reported lower results:
For both of these questions, Indigenous Veterans, Veterans who were visible minorities, CAF still serving, and younger Veterans (<60) reported lower levels of satisfaction than other Veterans.
|
September 30, 2026 June 30, 2027 |
Assistant Deputy Minister, Service Delivery in collaboration with ADM, Strategic Policy, Planning and Performance Assistant Deputy Minister, Strategic Policy, Planning and Performance |
Appendix A: Status update on the 2022 Office of the Auditor General's Processing Disability Benefits for Veterans audit report recommendations
Update on the 2022 Office of the auditor general's processing disability benefits for Veterans audit.
In 2022, the Office of the Auditor General of Canada conducted an audit of VAC's disability benefits processing. The report had four recommendations. Below are the recommendations and their status as of March 2024.
Recommendation 1 - Due Date: 31 December 2023 - Outstanding
Veterans Affairs Canada and the RCMP should work together to establish a formal costing process and determine the right level of funding needed for processing applications from RCMP Veterans in a timely manner.
This continues to be worked on and is expected to be completed in March 2024.
Recommendation 2 - Due Date: 30 April 2024 - Outstanding
To provide useful waiting-time information for Veterans, Veterans Affairs Canada should review the end date it uses to calculate the period under its service standard so that it can report consistently and accurately on its performance against this standard.
This recommendation has been partially implemented. As of 1 April 2022, the end date used to calculate the service standard was changed to include the time it takes from the date of decision to the date the payment amount is verified (for favourable decisions).
The second part that VAC is working on to support this recommendation pertains to a review of departmental service standards. This work is underway; however, it is not expected to be completed by the 30 April 2024 due date.
Recommendation 3 - Due Date: 31 March 2023 - Closed*
Veterans Affairs Canada should address weaknesses in the quality and organization of its data. This would allow the Department to better monitor the Disability Benefits program and use the data to inform decision making about efficiency improvements.
The Department has completed some work to address this recommendation; however, the evaluation team faced challenges with regards to the disability data, similar to the OAG auditors, as such further work is required.
*This recommendation was deemed complete, but issues remain.
Recommendation 4 - Due Date: 31 March 2023 - Closed*
Veterans Affairs Canada should work with central government agencies to establish a sustainable long - term resourcing plan for processing disability benefit applications in a timely manner. This plan should consider the number of applications the Department expects to receive and the efficiency it expects to gain from its process improvement initiatives.
The Department developed a plan to secure more permanent resources to reduce the processing times for individuals applying for DB; however, this plan was not funded in the federal budget 2023. Instead, in November 2023, the Minister of Veterans Affairs announced an extension of the temporary resources for an additional two years, from 1 April 2024 to 31 March. Further efforts are needed to ensure the resources are in place long-term to support the demand for the disability benefits program.
*This recommendation was deemed complete, but issues remain.
Appendix B - Service standards of other government departments
Employment and Social Development Canada - Canada Pension Plan Disability BenefitsFootnote 32
Application for Canada Pension Plan disability benefits
Standard: A decision is made within 120 calendar days of receiving a complete application
Target: To meet this standard 80% of the time
Performance in 2022 to 2023: ESDC met this standard 79% of the time
Canada Pension Plan disability benefit for applicants with a terminal illness
Standard: A decision is made within 5 business days of receiving a complete terminal illness application
Target: To meet this standard 95% of the time
Performance in 2022 to 2023: ESDC met this standard 91% of the time
Canada Pension Plan disability benefit for applicants with a grave medical condition
Standard: A decision is made within 30 calendar days of receiving a complete application if the individual has a grave medical condition
Target: To meet this standard 80% of the time
Performance in 2022 to 2023: ESDC met this standard 84.4% of the time
Canada Pension Plan disability benefit reconsiderations
Standard: A decision is made within 120 calendar days of receiving a request for reconsideration
Target: To meet this standard 80% of the time
Performance in 2022 to 2023: ESDC met this standard 62% of the time
Immigration, Refugees and Citizenship Canada
Permanent residence applications: the service standards apply only to applications with complete information and supporting documents.
Initial permanent resident card
Service standard: issue an initial permanent resident card within 60 days of confirming that a permanent residence form has been completed at a port of entry or at an IRCC inland office
Target: meet the standard for at least 80% of submitted applications
Performance in 2022-2023: processed 73% of applications within the standard
We introduced this service standard in April 2010 and reviewed it in February 2019.
Economic class
Canadian experience class (via Express Entry)
Service standard: process electronic applications within 180 days
Target: meet the standard for at least 80% of submitted applications (within the approved annual immigration levels plan)
Performance in 2022-2023: processed 85% of applications within the standard
We introduced this service standard in March 2015 and reviewed it in February 2019.
Federal Skilled Worker Program (via Express Entry)
Service standard: process electronic applications within 180 days
Target: meet the standard for at least 80% of submitted applications (within the approved annual immigration levels plan)
Performance in 2022-2023: processed 80% of applications within the standard
We introduced this service standard in March 2015 and reviewed it in February 2019.
Provincial Nominee Program (paper applications)
Service standard: process all paper applications within 11 months (which doesn't include the province or territory's processing time)
Target: meet the standard for at least 80% of submitted applications (within the approved annual immigration levels plan)
Performance in 2022-2023: processed 23% of applications within the standard
We introduced this service standard in September 2011 and reviewed it in February 2019.
Provincial Nominee Program (via Express Entry - Electronic applications)
Service standard: process electronic applications within 180 days (which doesn't include the province or territory's processing time)
Target: meet the standard for at least 80% of submitted applications (within the approved annual immigration levels plan)
Performance in 2022-2023: processed 70% of applications within the standard
We introduced this service standard in March 2015 and reviewed it in February 2019.
Quebec-selected skilled worker program
Service standard: process applications within 11 months (which doesn't include the province's processing time)
Target: meet the standard for at least 80% of submitted applications
Performance in 2022-2023: processed 48% of applications within the standard
We introduced this service standard in September 2011 and reviewed it in February 2019.
Federal Skilled Trades Program (via Express Entry)
Service standard: process electronic applications within 180 days (which doesn't include the province or territory's processing time)
Target: meet the standard for at least 80% of submitted applications (within the approved annual immigration levels plan)
Performance in 2022-2023: No applications were received within this past fiscal year
We introduced this service standard in March 2015 and reviewed it in February 2019.
Family sponsorship
Family Class Priority (Overseas - spouses, common-law partners, conjugal partners and dependent children)
Service standard: process applications within 12 months
Target: meet the standard for at least 80% of submitted applications
Performance in 2022-2023: processed 66% of applications within the standard
We introduced this service standard in April 2010.
Canada Revenue Agency
Tax returns
Individual income tax returns (T1) - digital
- What is this? This is a timeliness service standard for processing T1 individual income tax returns received electronically from individuals. Our standard applies to returns received on or before filing due dates and excludes returns filed for deceased, bankruptcy, international and non-resident individuals, and emigrants. It also does not apply in situations where returns are filed for multiple tax years, or contact must be made for more information. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice of assessment within two weeks of receiving your on-time filed digital individual income tax return.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022 filing season, 96% of the on-time filed digital T1 individual income tax returns received were processed within this standard.
Individual income tax returns (T1) - paper
- What is this? This is a timeliness service standard for processing paper T1 individual income tax returns from individuals. Our standard applies to returns received on or before filing due dates and excludes returns filed for deceased, bankruptcy, international and non-resident individuals, and emigrants. It also does not apply in situations where returns are filed for multiple tax years, or contact must be made for more information. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice of assessment within eight weeks of receiving your on-time filed paper individual income tax return.
- Our target: The CRA aims to meet this standard 95% of the time.
- COVID-19: Expect the normal timeframe to be extended to 10 to 12 weeks in most cases for processing paper T1 returns. For faster service, you can submit or re-submit your return electronically using NETFILE certified tax software. This does not include returns that must be filed by paper or are excluded from electronic filing.
- Our performance result: In the 2022 filing season, 98% of the on-time filed paper T1 individual income tax returns were processed within this standard.
Corporation income tax returns (T2) - digital
- What is this? This is a timeliness service standard for assessing T2 corporation income tax returns filed electronically from businesses and incorporated self-employed individuals. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice of assessment within six weeks of receiving your digital corporation income tax return.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 98% of notices were issued within the standard for T2 corporation income tax returns filed digitally.
GST/HST returns - digital
- What is this? This is a timeliness service standard for processing GST/HST returns filed electronically from businesses and self-employed individuals. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice of assessment, if applicable, within four weeks of receiving your digital GST/HST return.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 97% of notices were issued within the standard for GST/HST returns filed digitally.
T3 trust returns
- What is this? This is a timeliness service standard for processing T3 trust returns from trust recipients. A T3 income tax return is a form completed by a trustee to assess the tax liability of a trust. A T3 return is filed as both an income tax return (which calculates tax liability) and an information return (which reports amounts allocated and designated to beneficiaries). Our goal is to process T3 trust returns within seventeen weeks, which includes assessing the T3 return and mailing a notice of assessment and refund, if applicable. This service standard was modified in 2017-2018.
- Our standard: Our goal is to issue your notice of assessment within seventeen weeks of receiving your trust return.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 75% of T3 trust returns were processed within this standard. The CRA is refining the new T3 system to improve the result in 2023-2024.
T1 adjustment requests - routine - digital
- What is this? This is a timeliness service standard for responding to digital adjustment requests (T1) from individuals or their representatives. Our standard applies to straightforward taxpayer-requested adjustments only. Some change requests are considered complex and will take longer to process. Complex requests includes situations where additional information or review is required. This service standard was modified in 2019-2020.
- Our standard: Our goal is to issue your notice of reassessment or a letter of explanation within two weeks of receiving your digital request to change your individual income tax return.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 98% of these notices of reassessment were issued within this standard.
T1 adjustment requests - routine - paper or telephone
- What is this? This is a timeliness service standard for responding to paper or telephone adjustment requests (T1) from individuals or their representatives. Our standard applies to straightforward taxpayer-requested adjustments only. Some change requests are considered complex and will take longer to process. Complex requests includes situations where additional information or review is required. This service standard was modified in 2019-2020.
- Our standard: Our goal is to issue your notice of reassessment or a letter of explanation within eight weeks of receiving your paper or telephone request to change your individual income tax return.
- Our target: The CRA aims to meet this standard 95% of the time.
- COVID-19: Expect the normal timeframe to be extended to 10 to 12 weeks in most cases for processing T1 adjustments submitted by paper. For faster service you can submit your requests for changes electronically, using Change My Return in My Account or ReFILE.
- Our performance result: In the 2022-2023 fiscal year, 90% of these notices of reassessment were issued within this standard. The CRA is enhancing the processing of T1 adjustments in an endeavour to improve the result in 2023-2024.
Benefits
Benefit applications - digital
- What is this? This is a timeliness service standard for processing digital Canada child benefits applications. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice and payment, if applicable, within eight weeks of receiving your digital Canada child benefit application.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 92% of these digital benefit applications were processed within this standard. The Canada child benefit program experienced higher-than-expected volume of applications, affecting the CRA's ability to respond to digital application within the established service standard.
Benefit applications - paper
- What is this? This is a timeliness service standard for processing paper Canada child benefits applications. This service standard was modified in 2018-2019.
- Our standard: Our goal is to issue your notice and payment, if applicable, within eleven weeks of receiving your paper Canada child benefit application.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 90% of these paper benefit applications were processed within this standard. The Canada child benefit program experienced higher-than-expected volume of applications, affecting the CRA's ability to respond to paper applications within the established service standard.
Disability Tax Credit Certificate
- What is this? This is a timeliness service standard for processing Disability Tax Credit Certificates (T2201) from individuals or their representatives. Our standard applies to straightforward taxpayer-requested certificates only. Some requests are considered complex and will take longer to process. Complex requests includes situations where additional information or review is required. This service standard was modified in 2019-2020.
- Our standard: Our goal is to issue your Disability Tax Credit Certificate within eight weeks of receiving your request.
- Our target: The CRA aims to meet this standard 95% of the time.
- Our performance result: In the 2022-2023 fiscal year, 94% of these certificates were issued within this standard. The CRA is enhancing the processing of Disability Tax Credit Certificates in an endeavour to improve the result in 2023-2024.
Complex adjustment requests
Processing time frames apply to routine adjustment requests. Some change requests are considered complex and will take longer to process due to the additional verification required. They include adjustments related to:
- multiple tax returns
- tax years beyond the normal three-year reassessment period
- a bankruptcy return
- a deceased taxpayer
- a carry-back amount such as a capital or non-capital loss
- an international or non-resident client
- the elected split-pension amount
- a request from the CRA to you or your authorized representative for more information or documentation
- Processing your request is the CRA's highest priority. The time required to complete a complex adjustment request varies with the type of adjustment and the circumstances involved. The CRA continually strives to find the right balance between processing timeliness and the need to protect the integrity of the self-assessment tax system.