Entitlement Eligibility Guideline (EEG)
Date reviewed: 22 January 2025
Date created: February 2005
ICD-11 code: FB40.1
VAC medical code: 01328 Plantar fasciitis
This publication is available upon request in alternate formats.
Full document – PDF Version
Definition
Plantar fasciitis is a common cause of heel pain characterized by pain in the plantar heel with tenderness at the medial calcaneal tubercle and symptoms that are most noticeable with weight-bearing first thing in the morning or after a period of rest. The pain is often described as sharp, progressive pain and can radiate across the arch into the forefoot in severe cases.
For the purposes of this entitlement eligibility guideline (EEG), equivalent diagnoses to plantar fasciitis include:
- enthesopathy of the plantar fascia
- plantar fasciosis
- heel spur syndrome.
Diagnostic standard
A diagnosis from a qualified physician, nurse practitioner, or physician assistant (within their scope of practice) is required.
Plantar fasciitis is a clinical diagnosis made using history and physical examination with the following features:
- plantar heel pain most noticeable with initial steps after a period of inactivity, but also worse following prolonged weight bearing
- heel pain precipitated by a recent increase in weight bearing activity
- pain with palpation of the proximal insertion of the plantar fascia
- positive windlass test
- negative tarsal tunnel test
- limited active and passive talocrural joint dorsiflexion range of movement
- abnormal foot posture score
- high body mass index (BMI) in non-athletic individuals.
Imaging studies are usually not indicated for individuals that meet clinical examination criteria for plantar fasciitis until they fail conservative interventions. Refractory heel pain requires further diagnostic assessment, which may include some of the following studies:
- x-rays to look for bony lesions
- magnetic resonance imaging (MRI) to rule out soft tissue or bony lesions
- electromyography (EMG) for tarsal tunnel syndrome
- bone scans for stress fracture or bone infection
- computed tomography (CT) to evaluate for subtalar arthritis, calcaneal cyst, and stress fractures
- ankle-brachial index and pulse volume recording to evaluate for peripheral arterial disease.
Note: For Veterans Affairs Canada (VAC) purposes, relevant imaging may be provided, but is not required.
Anatomy and physiology
The plantar fascia is a strong fibrous band of tissue that extends from the plantar calcaneal tuberosity to the flexor tendon expansion in the forefoot (Figure 1: Plantar fasciitis). The plantar fascia comprises three segments originating from the hindfoot, providing essential arch support, and serving as a shock absorber. The windlass mechanism is a term used to describe the role of the plantar fascia in supporting the arch of the foot and refers to the concept that as the toes are dorsiflexed, the plantar fascia is stretched thereby accentuating the arch of the foot.
Figure 1: Plantar fasciitis
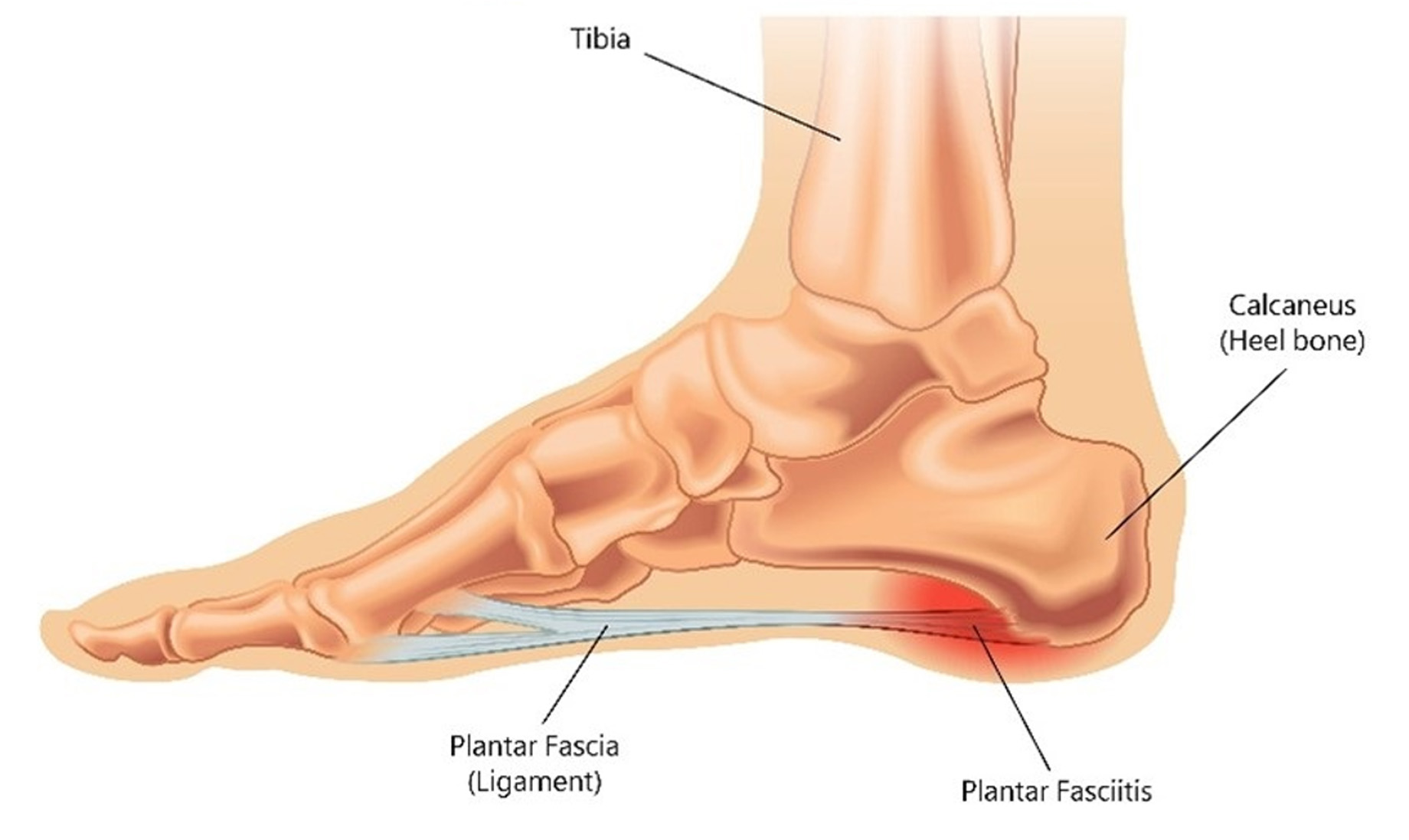
A side profile of the foot illustrates the tibia positioned above the ankle and the plantar fascia ligament stretching from the heel bone (calcaneus) to the ball of the foot. A highlighted area near the heel shows painful micro-tears in the plantar fascia, a common source of heel pain. Source: Veterans Affairs Canada (2024).
Plantar fasciitis is often an overuse injury primarily due to a repetitive strain causing micro-tears of the plantar fascia and can also occur due to trauma or other multifactorial causes (Figure 2: Torn plantar fascia). Calcaneal (heel) spurs are not uncommon findings in individuals with a history of plantar fasciitis and are not well correlated with plantar fasciitis symptoms. While heel spurs can occur with plantar fasciitis, they are not the cause.
Figure 2: Torn plantar fascia
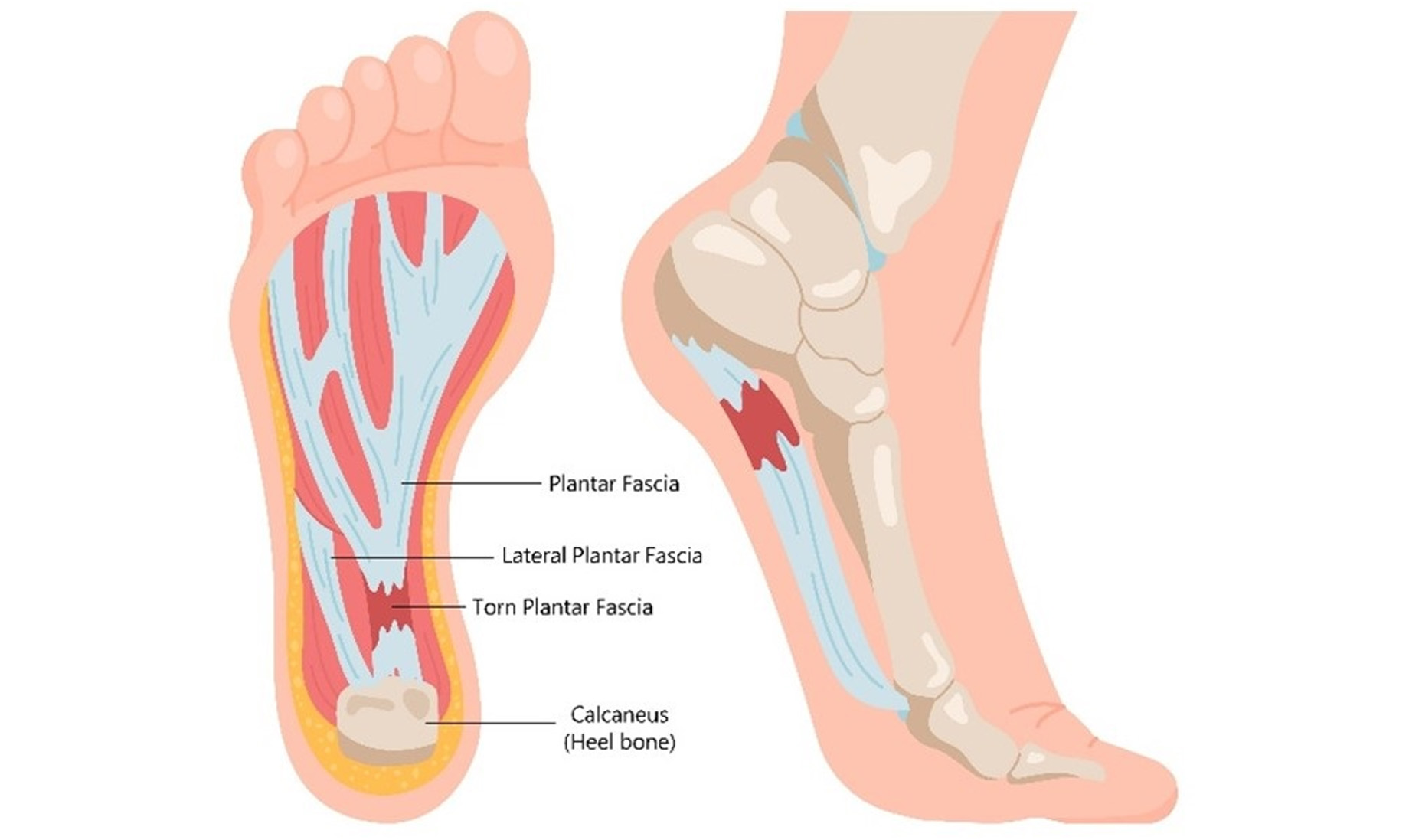
The underside of a human foot shows the lateral plantar fascia extending from the heel bone (calcaneus) to the ball of the foot. A red-highlighted area near the heel indicates torn fascia and inflammation, characteristic of plantar fasciitis. A side profile view also displays the inflamed fascia zone near the heel. Source: Veterans Affairs Canada (2024).
There are numerous risk factors for developing plantar fasciitis which can be simplified into overuse or repetitive trauma risk factors (running, sporting activities, training), mechanical risk factors (improper footwear, pronated foot, externally rotated foot, pes cavus), degenerative risk factors (age, heel fat pad atrophy), and inflammation (rheumatoid arthritis, systemic lupus erythematosus, gout, and ankylosing spondylitis).
Clinical features
The most prominent clinical feature of plantar fasciitis is pain in the anteromedial aspect of the heel that is often insidious in onset and progressive. The pain is usually acute when the individual first steps out of bed or initiates movement after a period of inactivity (also referred to as “start-up” pain). The pain may worsen as the day progresses, after periods of prolonged standing, and worsened when walking barefoot, on toes, or climbing stairs. Pain usually subsides with rest. Some people may experience burning, tingling, and a sharp pain in the heel. The discomfort can be anywhere on the sole of the foot.
On examination, pain is often localized to the anteromedial aspect of the heel on palpation. Mechanical changes in the foot such as pes planus (flat feet), pes cavus (high arches), tight Achilles tendon, or changes in the range of motion in the first ray of metatarsals, subtalar joint, or midtarsal joint may be noted.
Factors that can influence or trigger the onset of pain are foot structure (pes cavus or pes planus), overpronation, an excessive inward roll and collapse of the medial arch of the foot, tightness or weakness of the gastrocnemius, soleus, or Achilles tendon, excess weight, occupation, poorly fitting shoes, and sudden increases in activity or excessive training. Plantar fasciitis can resolve spontaneously with 80% of cases resolving within one year.
Plantar fasciitis is the most common cause of heel pain. Up to 15% of foot injuries in the general population and 17% of foot injuries in the running population are attributed to plantar fasciitis. Adults of all ages are affected with peaks between 40 and 60 years of age. Adult females present twice as often as males, while in younger individuals males and females are affected equally. One third of individuals experience plantar fasciitis bilaterally. Amongst military service members, female sex, black ethnicity, non-commissioned rank, and service in the army have been identified as risk factors for plantar fasciitis.
Entitlement considerations
In this section
Section A: Causes and/or aggravation
Section B: Medical conditions which are to be included in entitlement/assessment
Section A: Causes and/or aggravation
For VAC entitlement purposes, the following factors are accepted to cause or aggravate the conditions included in the Definition section of this EEG, and may be considered along with the evidence to assist in establishing a relationship to service. The factors have been determined based on a review of up-to-date scientific and medical literature, as well as evidence-based medical best practices. Factors other than those listed may be considered, however consultation with a disability consultant or medical advisor is recommended.
The timelines cited below are for guidance purposes. Each case should be adjudicated on the evidence provided and its own merits.
Factors
- Having experienced trauma to the plantar aspect of the affected foot prior to clinical onset or aggravation of plantar fasciitis. For trauma to cause or aggravate plantar fasciitis, the following should be evident:
- within seven days of the injury, development of tenderness, pain, swelling, discoloration, or altered mobility, or any other pertinent sign or symptom, should occur in the sole of the foot, and
- signs/symptoms should recur, either continuously or intermittently, from the time of the specific trauma to the time of diagnosis.
- Having a biomechanical abnormality of the foot at the time of clinical onset or aggravation of plantar fasciitis. Biomechanical abnormality means an injury or disease that has resulted in overpronation or under-pronation, or decreased ankle or forefoot flexibility. Examples include but are not limited to pes planus, pes cavus, tight Achilles tendon resulting in inadequate dorsiflexion, weakness of the plantar flexor musculature, and chronic foot pronation.
- Having a systemic arthritis prior to clinical onset or aggravation of plantar fasciitis, including but not limited to, the following:
- ankylosing spondylitis
- arthritis associated with inflammatory bowel disease
- psoriatic arthritis
- Reiter’s syndrome
- rheumatoid arthritis
- depositional arthritis (including gout and pseudogout).
- Having an overuse injury affecting the plantar aspect of the foot within two months of clinical onset or aggravation of plantar fasciitis. Overuse injuries involve the sole of the foot and are caused by an extraneous physical or mechanical force.
Examples of overuse injuries include:
- increasing frequency or intensity of running, jogging, or training
- participating in marching or foot drills
- undertaking activity involving repetitive or prolonged weight bearing
- increasing the frequency, duration, or intensity of weight bearing activity.
- Wearing ill-fitting footwear with inadequate cushioning during weight bearing exercise which involves the affected foot within seven days before the clinical onset or aggravation of plantar fasciitis.
- Having class 3/severe obesity (defined as body mass index [BMI] of 40 or greater) at the time of clinical onset or aggravation of plantar fasciitis.
- Inability to obtain appropriate clinical management of plantar fasciitis.
Section B: Medical conditions which are to be included in entitlement/assessment
Section B provides a list of diagnosed medical conditions which are considered for VAC purposes to be included in the entitlement and assessment of plantar fasciitis.
- Calcaneal (heel) spurs
- Flat foot
- Pes planus
- Chronic calcaneal bursitis
- Pes cavus
- Club foot
- Chronic foot strain/sprain
Section C: Common medical conditions which may result, in whole or in part, from plantar fasciitis and/or its treatment
No consequential medical conditions were identified at the time of the publication of this EEG. If the merits of the case and medical evidence indicate that a possible consequential relationship may exist, consultation with a disability consultant or medical advisor is recommended.
Links
Related VAC guidance and policy:
- Ankylosing Spondylitis – Entitlement Eligibility Guidelines
- Pes Planus - Entitlement Eligibility Guidelines
- Rheumatoid Arthritis – Entitlement Eligibility Guidelines
- Pain and Suffering Compensation – Policies
- Royal Canadian Mounted Police Disability Pension Claims – Policies
- Dual Entitlement – Disability Benefits – Policies
- Establishing the Existence of a Disability – Policies
- Disability Benefits in Respect of Peacetime Military Service – The Compensation Principle – Policies
- Disability Benefits in Respect of Wartime and Special Duty Service – The Insurance Principle – Policies
- Disability Resulting from a Non-Service Related Injury or Disease – Policies
- Consequential Disability – Policies
- Benefit of Doubt – Policies
References as of 22 January 2025
Arslan, I. G., Dijksma, I., van Etten-Jamaludin, F. S., Lucas, C., & Stuiver, M. M. (2021). Nonexercise Interventions for Prevention of Musculoskeletal Injuries in Armed Forces: A Systematic Review and Meta-Analysis. American Journal of Preventive Medicine, 60(2), e73–e84. https://doi.org/10.1016/j.amepre.2020.08.007
Australian Government, Repatriation Medical Authority. (2003). Statement of principles concerning plantar fasciitis, reasonable hypothesis, No 47 of 2003. SOPs - Repatriation Medical Authority
Australian Government, Repatriation Medical Authority. (2003). Statement of principles concerning plantar fasciitis, balance of probabilities, No 48 of 2003. SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. Statement of Principles concerning plantar fasciitis (Balance of Probabilities) (No. 83 of 2023). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. Statement of Principles concerning plantar fasciitis (Reasonable Hypothesis) (No. 82 of 2023). SOPs - Repatriation Medical Authority
Baxter, M. L., Baycroft, C., & Baxter, G. D. (2011). Lower Limb Injuries in Soldiers: Feasibility of Reduction Through Implementation of a Novel Orthotic Screening Protocol. Military Medicine, 176(3), 291–296. https://doi.org/10.7205/MILMED-D-10-00352
Bonanno, D. R., Murley, G. S., Munteanu, S. E., Landorf, K. B., & Menz, H. B. (2018). Effectiveness of foot orthoses for the prevention of lower limb overuse injuries in naval recruits: A randomised controlled trial. British Journal of Sports Medicine, 52(5), 298–302. https://doi.org/10.1136/bjsports-2017-098273
Bracker, M. D. (2012). The 5-Minute Sports Medicine Consult: Second Edition. Buchanan, B. K., Sina, R. E., & Kushner, D. (2024). Plantar Fasciitis. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK431073/
Butterworth, P. A., Landorf, K. B., Smith, S. E., & Menz, H. B. (2012). The association between body mass index and musculoskeletal foot disorders: A systematic review. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 13(7), 630–642. https://doi.org/10.1111/j.1467-789X.2012.00996.x
Carden, P. P. J., Izard, R. M., Greeves, J. P., Lake, J. P., & Myers, S. D. (2015). Force and acceleration characteristics of military foot drill: Implications for injury risk in recruits. BMJ Open Sport & Exercise Medicine, 1(1), bmjsem-2015-000025. https://doi.org/10.1136/bmjsem-2015-000025
Choudhary, R., & Kunal, K. (2021). Modifiable Risk Factors of Plantar Fasciitis in Non- Athletic Patients and Proposal of a New Objective Assessment System— RKISP. Revista Brasileira De Ortopedia, 56(3), 368–371. https://doi.org/10.1055/s-0040-1716762
Fenn, B. P., Song, J., Casey, J., Waryasz, G. R., DiGiovanni, C. W., Lubberts, B., & Guss, D. (2021). Worldwide epidemiology of foot and ankle injuries during military training: A systematic review. BMJ Military Health, 167(2), 131–136. https://doi.org/10.1136/bmjmilitary-2020-001591
Flores, D. V., Goes, P. K., Damer, A., & Huang, B. K. (2024). The Heel Complex: Anatomy, Imaging, Pathologic Conditions, and Treatment. RadioGraphics, 44(4), e230163. https://doi.org/10.1148/rg.230163
Franklyn-Miller, A., Bilzon, J., Wilson, C., & McCrory, P. (2014). Can RSScan footscan(®) D3DTM software predict injury in a military population following plantar pressure assessment? A prospective cohort study. Foot (Edinburgh, Scotland), 24(1), 6–10. https://doi.org/10.1016/j.foot.2013.11.002
Franklyn-Miller, A., Wilson, C., Bilzon, J., & McCrory, P. (2011). Foot orthoses in the prevention of injury in initial military training: A randomized controlled trial. The American Journal of Sports Medicine, 39(1), 30–37. https://doi.org/10.1177/0363546510382852
Fraser, J. J., Pommier, R., MacGregor, A. J., Silder, A., & Sander, T. C. (2022). Does policy that provides choice in athletic footwear affect musculoskeletal injury risk in US Coast Guard recruits? BMJ Military Health, e002211. https://doi.org/10.1136/military-2022-002211
Fredette, M. A., Roy, J.-S., Esculier, J.-F. O., & Perreault, K. (2021). Most Military Runners Report Recent Changes in Running Parameters Before Lower Limb Injury Onset. Military Medicine, 186(11–12), e1140–e1148. https://doi.org/10.1093/milmed/usaa524
Glazer, J. L. (2009). An approach to the diagnosis and treatment of plantar fasciitis. The Physician and Sportsmedicine, 37(2), 74–79. https://doi.org/10.3810/psm.2009.06.1712
Hamstra-Wright, K. L., Huxel Bliven, K. C., Bay, R. C., & Aydemir, B. (2021). Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis. Sports Health, 13(3), 296–303. https://doi.org/10.1177/1941738120970976
Harutaichun, P., Boonyong, S., & Pensri, P. (2019). Predictors of plantar fasciitis in Thai novice conscripts after 10-week military training: A prospective study. Physical Therapy in Sport: Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 35, 29–35. https://doi.org/10.1016/j.ptsp.2018.10.004
Harutaichun, P., Boonyong, S., & Pensri, P. (2021). Differences in lower-extremity kinematics between the male military personnel with and without plantar fasciitis. Physical Therapy in Sport: Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 50, 130–137. https://doi.org/10.1016/j.ptsp.2021.04.007
Hawke, F., Burns, J., Radford, J. A., & du Toit, V. (2008). Custom-made foot orthoses for the treatment of foot pain. The Cochrane Database of Systematic Reviews, 3, CD006801. https://doi.org/10.1002/14651858.CD006801.pub2
Helton, G. L., Cameron, K. L., Zifchock, R. A., Miller, E., Goss, D. L., Song, J., & Neary, M. T. (2019). Association Between Running Shoe Characteristics and Lower Extremity Injuries in United States Military Academy Cadets. The American Journal of Sports Medicine, 47(12), 2853–2862. https://doi.org/10.1177/0363546519870534
Irving, D. B., Cook, J. L., Young, M. A., & Menz, H. B. (2007). Obesity and pronated foot type may increase the risk of chronic plantar heel pain: A matched case- control study. BMC Musculoskeletal Disorders, 8, 41. https://doi.org/10.1186/1471-2474-8-41
Kakouris, N., Yener, N., & Fong, D. T. P. (2021). A systematic review of running-related musculoskeletal injuries in runners. Journal of Sport and Health Science, 10(5), 513–522. https://doi.org/10.1016/j.jshs.2021.04.001
Kelly, J. L., & Valier, A. R. (2018). The Use of Orthotic Insoles to Prevent Lower Limb Overuse Injuries: A Critically Appraised Topic. Journal of Sport Rehabilitation, 27(6), 591–595. https://doi.org/10.1123/jsr.2016-0142
Khired, Z., Najmi, M. H., Akkur, A. A., Mashhour, M. A., & Bakri, K. A. (2022). The Prevalence and Risk Factors of Plantar Fasciitis Amongst the Population of Jazan. Cureus, 14(9), e29434. https://doi.org/10.7759/cureus.29434
Kibler, W. B., Herring, S. A., & Press, J. M. (Eds.). (1998). Functional rehabilitation of sports and musculoskeletal injuries. Aspen.
Klein, S. E., Dale, A. M., Hayes, M. H., Johnson, J. E., McCormick, J. J., & Racette, B. A. (2012). Clinical presentation and self-reported patterns of pain and function in patients with plantar heel pain. Foot & Ankle International, 33(9), 693–698. https://doi.org/10.3113/FAI.2012.0693
Knobloch, K., Yoon, U., & Vogt, P. M. (2008). Acute and overuse injuries correlated to hours of training in master running athletes. Foot & Ankle International, 29(7), 671–676. https://doi.org/10.3113/FAI.2008.0671
Koc, T. A., Bise, C. G., Neville, C., Carreira, D., Martin, R. L., & McDonough, C. M. (2023). Heel Pain - Plantar Fasciitis: Revision 2023. The Journal of Orthopaedic and Sports Physical Therapy, 53(12), CPG1–CPG39. https://doi.org/10.2519/jospt.2023.0303
Labovitz, J. M., Yu, J., & Kim, C. (2011). The role of hamstring tightness in plantar fasciitis. Foot & Ankle Specialist, 4(3), 141–144. https://doi.org/10.1177/1938640010397341
Latt, L. D., Jaffe, D. E., Tang, Y., & Taljanovic, M. S. (2020). Evaluation and Treatment of Chronic Plantar Fasciitis. Foot & Ankle Orthopaedics, 5(1), 2473011419896763. https://doi.org/10.1177/2473011419896763
Littlejohn, B. (2024). From Heel to Toe: Investigating Plantar Fasciitis Causes, Diagnosis, and Treatment Strategies. Digital Commons.
Lopes, A. D., Hespanhol Júnior, L. C., Yeung, S. S., & Costa, L. O. P. (2012). What are the main running-related musculoskeletal injuries? A Systematic Review. Sports Medicine (Auckland, N.Z.), 42(10), 891–905. https://doi.org/10.1007/BF03262301
Lotke, P. A., Abboud, J. A., & Ende, J. (2014). Lippincott’s primary care orthopaedics (2nd edition, 1–1 ressource en ligne : illustrations en partie en couleur). Lippincott Williams & Wilkins; WorldCat.
Lovalekar, M., Johnson, C. D., Eagle, S., Wohleber, M. F., Keenan, K. A., Beals, K., Nindl, B. C., & Connaboy, C. (2018). Epidemiology of musculoskeletal injuries among US Air Force Special Tactics Operators: An economic cost perspective. BMJ Open Sport & Exercise Medicine, 4(1), e000471. https://doi.org/10.1136/bmjsem-2018-000471
Mahmood, S., Huffman, L. K., & Harris, J. G. (2010). Limb-length discrepancy as a cause of plantar fasciitis. Journal of the American Podiatric Medical Association, 100(6), 452–455. https://doi.org/10.7547/1000452
Mansur, H., Ferreira, G. F., Ferreira-Junior, J. B., de Araújo, B. A. S., & Maranho, D. A. (2024). Leg length discrepancy is not a risk factor for plantar fasciitis. Archives of Orthopaedic and Trauma Surgery, 144(4), 1485–1490. https://doi.org/10.1007/s00402-024-05197-6
Martin, R. L., Davenport, T. E., Reischl, S. F., McPoil, T. G., Matheson, J. W., Wukich, D. K., McDonough, C. M., Altman, R. D., Beattie, P., Cornwall, M., Davis, I., DeWitt, J., Elliott, J., Irrgang, J. J., Kaplan, S., Paulseth, S., Torburn, L., Zachazewski, J., & Godges, J. J. (2014). Heel Pain—Plantar Fasciitis: Revision 2014. Journal of Orthopaedic & Sports Physical Therapy, 44(11), A1–A33. https://doi.org/10.2519/jospt.2014.0303
Mattila, V. M., Sillanpää, P. J., Salo, T., Laine, H.-J., Mäenpää, H., & Pihlajamäki, H. (2011). Can orthotic insoles prevent lower limb overuse injuries? A randomized- controlled trial of 228 subjects. Scandinavian Journal of Medicine & Science in Sports, 21(6), 804–808. https://doi.org/10.1111/j.1600-0838.2010.01116.x
Nesterovica, D., Vaivads, N., & Stepens, A. (2021). Relationship of footwear comfort, selected size, and lower leg overuse injuries among infantry soldiers. BMC Musculoskeletal Disorders, 22(1), 952. https://doi.org/10.1186/s12891-021-04839-9
Nesterovica, D., Vaivads, N., & Stepens, A. (2023). Increased Barefoot Stride Variability Might Be Predictor Rather than Risk Factor for Overuse Injury in the Military. International Journal of Environmental Research and Public Health, 20(15), 6449. https://doi.org/10.3390/ijerph20156449
Noriega, D. C., Cristo, Á., León, A., García-Medrano, B., Caballero-García, A., & Córdova- Martinez, A. (2022). Plantar Fasciitis in Soccer Players-A Systemic Review. International Journal of Environmental Research and Public Health, 19(21), 14426. https://doi.org/10.3390/ijerph192114426
Orr, R., Maupin, D., Palmer, R., Canetti, E. F. D., Simas, V., & Schram, B. (2022). The Impact of Footwear on Occupational Task Performance and Musculoskeletal Injury Risk: A Scoping Review to Inform Tactical Footwear. International Journal of Environmental Research and Public Health, 19(17), 10703. https://doi.org/10.3390/ijerph191710703
Owens, B. D., Wolf, J. M., Seelig, A. D., Jacobson, I. G., Boyko, E. J., Smith, B., Ryan, M. A. K., Gackstetter, G. D., Smith, T. C., & Millennium Cohort Study Team. (2013). Risk Factors for Lower Extremity Tendinopathies in Military Personnel. Orthopaedic Journal of Sports Medicine, 1(1), 2325967113492707. https://doi.org/10.1177/2325967113492707
Paradise, S. L., Beer, J. R., Cruz, C. A., Fechner, K. M., MacGregor, A. J., & Fraser, J. J. (2024). Prescribed footwear and orthoses are not prophylactic in preventing lower extremity injuries in military tactical athletes: A systematic review with meta-analysis. BMJ Military Health, 170(1), 64–71. https://doi.org/10.1136/bmjmilitary-2021-001955
Pasquina, P. F., Griffin, S. C., Anderson-Barnes, V. C., Tsao, J. W., & O’Connor, F. G. (2013). Analysis of injuries from the Army Ten Miler: A 6-year retrospective review. Military Medicine, 178(1), 55–60. https://doi.org/10.7205/milmed-d-11-00447
Pereira-Barriga, M. C., Borrero-Hernández, J. M., García-Iglesias, J. J., López-López, D., Ruiz-Frutos, C., Allande-Cussó, R., & Gómez-Salgado, J. (2024). A review of the injuries caused by occupational footwear. Occupational Medicine (Oxford, England), 74(3), 218–224. https://doi.org/10.1093/occmed/kqae003
Pohl, M. B., Hamill, J., & Davis, I. S. (2009). Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine, 19(5), 372–376. https://doi.org/10.1097/JSM.0b013e3181b8c270
Rhim, H. C., Kwon, J., Park, J., Borg-Stein, J., & Tenforde, A. S. (2021). A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life (Basel, Switzerland), 11(12), 1287. https://doi.org/10.3390/life11121287
Riddle, D. L., Pulisic, M., Pidcoe, P., & Johnson, R. E. (2003). Risk factors for Plantar fasciitis: A matched case-control study. The Journal of Bone and Joint Surgery. American Volume, 85(5), 872–877. https://doi.org/10.2106/00004623-200305000-00015
Robinson, M., Siddall, A., Bilzon, J., Thompson, D., Greeves, J., Izard, R., & Stokes, K. (2016). Low fitness, low body mass and prior injury predict injury risk during military recruit training: A prospective cohort study in the British Army. BMJ Open Sport & Exercise Medicine, 2(1), e000100. https://doi.org/10.1136/bmjsem-2015-000100
Ross, J. (1993). A review of lower limb overuse injuries during basic military training. Part 1: Types of overuse injuries. Military Medicine, 158(6), 410–415.
Sahin, N., Oztürk, A., & Atıcı, T. (2010). Foot mobility and plantar fascia elasticity in patients with plantar fasciitis. Acta Orthopaedica Et Traumatologica Turcica, 44(5), 385–391. https://doi.org/10.3944/AOTT.2010.2348
Scher, D., Belmont, P. J., & Owens, B. D. (2010). The Epidemiology of Plantar Faciitis. Lower Extremity Review.
Scher, D. L., Belmont, P. J., Bear, R., Mountcastle, S. B., Orr, J. D., & Owens, B. D. (2009). The incidence of plantar fasciitis in the United States military. The Journal of Bone and Joint Surgery. American Volume, 91(12), 2867–2872. https://doi.org/10.2106/JBJS.I.00257
Schoenfeld, A. J., Blauwet, C. A., & Katz, J. N. (Eds.). (2021). Principles of Orthopedic Practice for Primary Care Providers. Springer International Publishing. https://doi.org/10.1007/978-3-030-74625-4
Sobhani, S., Dekker, R., Postema, K., & Dijkstra, P. U. (2013). Epidemiology of ankle and foot overuse injuries in sports: A systematic review. Scandinavian Journal of Medicine & Science in Sports, 23(6), 669–686. https://doi.org/10.1111/j.1600-0838.2012.01509.x
Speed, C., Hazleman, B., & Dalton, S. (2006). Fast Facts: Soft Tissue Disorders. S. Karger AG. https://doi.org/10.1159/isbn.978-1-905832-27-9
Sung, K.-C., Chung, J.-Y., Feng, I.-J., Yang, S.-H., Hsu, C.-C., Lin, H.-J., Wang, J.-J., & Huang, C.-C. (2020). Plantar fasciitis in physicians and nurses: A nationwide population-based study. Industrial Health, 58(2), 153–160. https://doi.org/10.2486/indhealth.2019-0069
Taanila, H., Suni, J. H., Kannus, P., Pihlajamäki, H., Ruohola, J.-P., Viskari, J., & Parkkari, J. (2015). Risk factors of acute and overuse musculoskeletal injuries among young conscripts: A population-based cohort study. BMC Musculoskeletal Disorders, 16, 104. https://doi.org/10.1186/s12891-015-0557-7
Tenforde, A. S., Sayres, L. C., McCurdy, M. L., Collado, H., Sainani, K. L., & Fredericson, M. (2011). Overuse injuries in high school runners: Lifetime prevalence and prevention strategies. PM & R: The Journal of Injury, Function, and Rehabilitation, 3(2), 125–131; quiz 131. https://doi.org/10.1016/j.pmrj.2010.09.009
Thomas, J. L., Christensen, J. C., Kravitz, S. R., Mendicino, R. W., Schuberth, J. M., Vanore, J. V., Weil, L. S., Zlotoff, H. J., Bouché, R., & Baker, J. (2010). The Diagnosis and Treatment of Heel Pain: A Clinical Practice Guideline–Revision 2010. The Journal of Foot and Ankle Surgery, 49(3), S1–S19. https://doi.org/10.1053/j.jfas.2010.01.001
Umar, H., Idrees, W., Umar, W., Khalil, A., & Rizvi, Z. A. (2022). Impact of routine footwear on foot health: A study on plantar fasciitis. Journal of Family Medicine and Primary Care, 11(7), 3851–3855. https://doi.org/10.4103/jfmpc.jfmpc_637_21
Veterans Affairs Canada (2024). Plantar Fasciitis. License purchased for use from https://www.123rf.com/photo_201620631_plantar-fasciitis-plantar-fascia-inflammation-or-tearing-disorder.html
Veterans Affairs Canada (2024). Torn Plantar Fascia. License purchased for use from https://www.123rf.com/photo_82435631_plantar-fascitis.html
Waclawski, E. R., Beach, J., Milne, A., Yacyshyn, E., & Dryden, D. M. (2015). Systematic review: Plantar fasciitis and prolonged weight bearing. Occupational Medicine (Oxford, England), 65(2), 97–106. https://doi.org/10.1093/occmed/kqu177
Wardle, S. L., & Greeves, J. P. (2017). Mitigating the risk of musculoskeletal injury: A systematic review of the most effective injury prevention strategies for military personnel. Journal of Science and Medicine in Sport, 20 Suppl 4, S3– S10. https://doi.org/10.1016/j.jsams.2017.09.014
Werner, R. A., Gell, N., Hartigan, A., Wiggerman, N., & Keyserling, W. M. (2010). Risk factors for plantar fasciitis among assembly plant workers. PM & R: The Journal of Injury, Function, and Rehabilitation, 2(2), 110–116; quiz 1 p following 167. https://doi.org/10.1016/j.pmrj.2009.11.012
Whittle, R. S. (2022). Distance travelled by military recruits during basic training is a significant risk factor for lower limb overuse injury. BMJ Military Health, 168(5), 343–348. https://doi.org/10.1136/bmjmilitary-2020-001445
World Health Organization. (2022). ICD-11: International classification of diseases (11th revision). https://icd.who.int/
Yoon, Y. S., An, D. H., Lee, Y. J., Lee, D. Y., & Kyung, M. G. (2024). Comparison of in-shoe plantar pressure between Korean combat boots and running shoes. BMJ Military Health, e002592. https://doi.org/10.1136/military-2023-002592